POWERPLUSWATERMARKOBJECT29114390 INTRODUCTION REGIONAL ANESTHESIA OF THE NERVES OF THE
POWERPLUSWATERMARKOBJECT29114390 INTRODUCTION REGIONAL ANESTHESIA OF THE NERVES OF THE
Scalp Blocks and Conscious Sedation


Introduction
Regional anesthesia of the nerves of the scalp is referred to as “scalp block”. It has special relevance in neurosurgery where it has a role in stabilizing intraoperative hemodynamic response, which results from noxious stimuli. The technique serves to decrease the amount of general anesthetics used, which offers the opportunity for “awake craniotomies” and greater safety in patients with certain types of brain injury. In addition, it provides excellent post-operative relief from severe pain, both immediately as well as months after surgery.
Indications for Scalp Block (Adult and Pediatric)
1. Craniotomy - Several reflexogenic events occur during a craniotomy: insertion of the cranial pins of the head holder, incision of the scalp, craniotomy, and dural incision. Scalp blocks aim to blunt the hemodynamic reactions associated with all these events (HR stability and only very little variation in BP during the various stages of craniotomy, eventually preventing the rise of ICP)
2.) Analgesia for surgical drainage of chronic subdural hematoma (which requires no head-pinning)
3.) Mgt. of Post-op pain – Acute and Chronic Pain
Acute – immediately following craniotomy
Chronic Pain - Batoz et al found that postsurgical scalp infiltration with ropivacaine resulted in significantly lower pain levels both 24 hrs as well as 2 months post-operative.
This encourages us to investigate the possibility of perioperative scalp blocks providing acute as well as long-term pain relief. Newer drug forms of anesthetics with slow-releasing doses are currently being investigated.
4.) Headaches – cluster, cervicogenic, possibly migraines (occipital blocks)
5.) Neuralgias and neuropathies – occipital, post-herpetic etc.
6.) Any surgery (elective/emergency) involving scalp incisions – the appropriate anatomical blocks are used –
i) Any repair of lacerations in the face region – valuable for cosmetic regions, because a local field block can cause anatomical distortions, which can heal with imperfections.
ii) Nasal fracture (Supratrochlear block in addition to nasal block)
iii) Surgery of earlobes, occipital scalp wounds
iv) During ventriculo-peritoneal shunts
v) Surgical drainage of chronic subdural hematoma
vi) Surgery of forehead /upper eyelid: supraorbital + supratrochlear block
Anatomy of Scalp Nerves – Brief Review
The scalp has 5 layers: Skin (outermost), Connective tissue (contains some scalp vessels and a rich nerve supply), Aponeurosis galea (extending from the frontalis muscle anteriorly to the occipitalis muscle posteriorly), Loose connective tissue (which contains the major blood vessels) and lastly, the Periosteum (innermost). Scalp block provides regional anesthesia to all the 5 layers. The internal periosteum and the dura, innervated by nerves satellites of the meningeal vessels, are not blocked by this infiltration. Anteriorly the scalp is innervated by – 1. Supraorbital and 2. Supratrochlear nerves (derived from ophthalmic division of the trigeminal nerve.
Posteriorly – 1. Greater Occipital Nerve (derived from dorsal ramus of C2) and by 2. Lesser Occipital Nerve (ventral ramus of C2)
Lateral / temporo-parietal surfaces of the scalp – 1. Zygomaticotemporal (from maxillary division of the trigeminal nerve), 2. Auriculotemporal (from mandibular division), 3. Posterior auricular (facial nv) +Great Auricular nvs (cervical).
Surgical Landmarks of Scalp Blocks and Method-
1. Supraorbital – Supraorbital notch is palpated by finger along the superior orbital rim, and needle is inserted approx. 1 cm medial to the foramen, with a medial direction to avoid the penetration of the foramen at all costs (causes nervous trauma). Classically, the puncture point is in line with the centered pupil, just above the orbital ledge. Adult – 2ml (x2), children – 1-1.5 ml (x2)
2. Supratrochlear – Medially extending the supraorbital block, approx. 1 finger-breath medial to the S/O block – above the orbital ledge. Adults 1ml (x2); Children – 0.5 ml. (x2)
Alternatively, around the glabellar region, in the midline. Caution: intravascular injection of the angular vein. Adults 2 ml (x1); Children – 1 ml. (x1)
3. Zygomaticotemporal – 1 cm lateral and superior to lateral canthus of eye. Approx. lateral to the orbital margin, where the eyebrow ends. Adults 2ml (x2), Children 1ml (x2).
4. Auriculotemporal – Innervating the front of the ear and temples. The puncture pt. is in front of the tragus, directed laterally. When needle hits bone (deep) 2 ml, withdraw needle superficially and inject 2 ml again.Total 4ml (x2) in adults.
5. Posterior Temporal + Great Auricular – Both these nerves can be blocked together by injecting along the posterior border of upper 1/3rd of Sternocleidomastoid muscle.
The specific posterior auricular block is along the line of tragus, posterior to the ear. It blocks the region mainly behind the ear, as well as below it. Adults 2 ml (x2). The Great Auricular Nerve supplies below and behind the ear as well, but the region is more inferior relative to the P/T nv.
These two nerve blocks are especially important during placement of the DBS battery and extension wires.
6. Greater occipital nerve and lesser occipital nerves: – During head pinning before craniotomy, position the needle as close to the pins as possible, with care not to compromise the occipital artery. Can be injected as a fan block along occipital ridge to cover both GON and LON areas. Largest vol. of anesthetics is used – 5-6 ml in adults (x2), 2-4 ml in children. (x2). The best landmark is to palpate the occipital artery (if possible) and inject medially after careful aspiration.
Anesthetic Agents-
0.5 % bupivacaine with epinephrine (0.125 % in children) is widely used.
Complications –
1. Nervous - The only notorious accidents are the extension of the anesthesia to the motor nerves: facial droop, ptosis of superior eyelid; these incidents will gradually resolve as block wears off.
2. Vascular - The facial vascular richness poses major risk of vascular breach, with an intense and fast resorption of the anesthetic solution and the possibility of an intravascular injection. All the nerves are accompanied by an artery or close to a significant arterial axis; only the maxillary nerve is above the vessels.
With the supratrochlear nerve, it is possible to puncture the angular vein resulting in a hematoma in the surgery zone.
3. Articular - IM injection of the pterygoid muscles can involve a blocking of TMJ with limited oral opening and trismus.
Pediatric Population – Special Considerations
Largely similar to that in adult patients. Amounts of anesthetics are reduced.
Brief History
Special thanks to Dr. Dung Q. Tran of Georgetown University for his invaluable insights and contribution.
Girvin JP. Neurosurgical considerations and general methods for craniotomy under local anesthesia. Int Anesthiol Clin. 1986;24:89-114.
Pinowsky ML, Fishman FL, Reeves ST, et al. The effect of bupivacaine skull block on the hemodynamic response to craniotomy. Anesth Analg 1996;83:1256-1261.
Nguyen A, Girard F, et al. Scalp nerve blocks decrease the severity of pain after craniotomy Anesth Analg. 2001;93:12-72-1276.
Osborn IP, Sebeo J. “Scalp Block” during craniotomy: A classic technique revisited. J Neurosurg Anesthesiol 2010;22:187-194.
Tags: anesthesia of, the anesthesia, regional, powerpluswatermarkobject29114390, introduction, anesthesia, nerves
- NA OSNOVI 6 7 IN 30 ČLENA STATUTA SLOVENSKEGA
- LUNES 26 DE AGOSTO DE 2019 DIARIO OFICIAL 207
- EL MAPA REPRESENTA LA DISTRIBUCIÓN DE LAS TEMPERATURAS MEDIAS
- CARTA DELLE COLLEZIONI PRESENTAZIONE LA CARTA DELLE COLLEZIONI È
- 21 CONGRESO DE LA ASOCIACIÓN ESPAÑOLA DE ABOGADOS ESPECIALIZADOS
- CHARITY OFFICERS THE CHAIR AND TREASURER SOME
- ZAŁĄCZNIK NR 1 DO ZARZĄDZENIA NR …………… WÓJTA GMINY
- WRITTEN STATEMENT BY THE WELSH GOVERNMENT
- BIJGEWERKT TM NR 12 (NOTA VAN WIJZIGING DD 11
- WORKERS’ COMPENSATION CLAIM PROCEDURES SUPERVISOR’S NOTES WHEN AN EMPLOYEE
- PISTAS DE APLICACIÓN DE LA TEORÍA DE LAS INTELIGENCIAS
- 29 PERATURAN WALIKOTA MADIUN NOMOR 44
- WORKERS’ COMPENSATION DIVISION WORKER REQUEST FOR RECONSIDERATION THERE CAN
- THỨ HAI NGÀY 142013 CNXD ĐỌC CÓ ĂN BỚT
- AGRICULTURAL LABOUR AND UNFREEDOM SIRI WORKERS IN A VILLAGE
- DOBBS FERRY SCHOOLS CLOSED CNS CLOSED EFFECTIVE 102920 DOBBS
- SOUTENANCES DE THÈSES LE JEUNE KARINE UNE HISTOIRE
- MULTICOLUMN WATER TANK CONSTRUCTION SPECIFICATIONS TANK CONTRACTOR PHOENIX FABRICATORS
- CICLO FORMATIVO 20122013 CUIDADOS PALIATIVOS OBJETIVOS ACTIVIDAD PRÁCTICA 1
- KEEPING SALT OUT OF THE MURRAY SALT INTERCEPTION SCHEMES
- CICLO SEMINARIOS ESPECIALIZADOS CHILE DIGITAL 20132014 PROGRAMA Y FICHA
- EN ESTOS TIEMPOS LA DOCTRINA DE LOS BAUTISMOS ES
- COVENTRY SCHOOLS FORUM CONSTITUTION 1 PURPOSE OF THE SCHOOLS
- WARNING OF RIGHT COUNSEL STATE OF TEXAS COUNTY OF
- DATUM SIDA 20051104 0 (1) KOMMUNALT FÖRLUSTANSVAR KFA FÖR
- GTBTW265REV1 PÁGINA 3 ORGANIZACIÓN MUNDIAL DEL COMERCIO GTBTW265REV1 23
- HAYS COUNTY COMMISSIONERS COURT MINUTES MARCH 9
- SOPOT 20181120 INFORMACJA Z OTWARCIA OFERT DOT PRZETARGU NIEOGRANICZONEGO
- MEDIMED 19TH EDITION THE EUROMEDITERRANEAN DOCUMENTARY MARKET SITGES
- 10H00 10H20 ACCUEIL – CAFÉ SALLE S001 AU
WSPÓŁCZYNNIKI PRZELICZENIOWE DLA CENY DREWNA WIELKOWYMIAROWEGO SORTYMENT GATUNEK WSPÓŁCZYNNIK
NORTH MUNSTER UNDER 13 LEAGUE 2010 2011 SECTION
 18 JUAN J GARCÍA PELLICER JOSÉ V GARCÍA JIMÉNEZ
18 JUAN J GARCÍA PELLICER JOSÉ V GARCÍA JIMÉNEZDR HENRYK SUCHOJAD BIBLIOTEKA GŁÓWNA UNIWERSYTETU HUMANISTYCZNOPRZYRODNICZEGO JANA KOCHANOWSKIEGO
 UNMIK IPVQ PROVISIONAL INSTITUTIONS OF SELFGOVERNMENT INSTITUCIONET E PËRKOHSHME
UNMIK IPVQ PROVISIONAL INSTITUTIONS OF SELFGOVERNMENT INSTITUCIONET E PËRKOHSHMEPROTOKÓŁ NR 314 Z POSIEDZENIA ZARZĄDU „LOKALNEJ GRUPY RYBACKIEJ
 SISAK 3 LISTOPADA 2009 DOM KULTURE „KRISTALNA KOCKA VEDRINE“
SISAK 3 LISTOPADA 2009 DOM KULTURE „KRISTALNA KOCKA VEDRINE“AL COMUNE DI VALDIDENTRO PZA IV NOVEMBRE N 5
SEARCHING FOR STUDIES USEFUL LINKS NATIONAL AND REGIONAL
EXTRACT COMMENTS PROGRAM GETRNO PROG NAME GETRNO FILE
REIAL DECRET 15132006 DE 7 DE DESEMBRE PEL QUAL
OGŁOSZENIE Z DNIA 6 WRZEŚNIA 2019 R W SPRAWIE
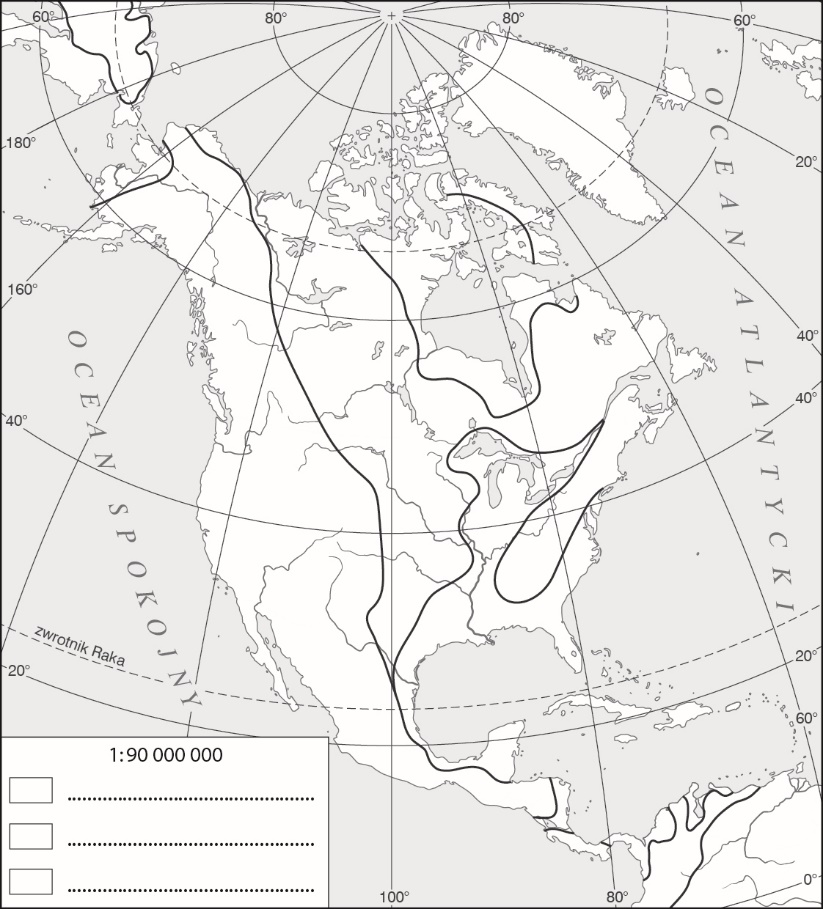 GEOGRAFIA KLASA VIII 06042020 TEMAT STANY ZJEDNOCZONE AMERYKI –
GEOGRAFIA KLASA VIII 06042020 TEMAT STANY ZJEDNOCZONE AMERYKI –2 GOBIERNO DE PUERTO RICO 18VA ASAMBLEA 1RA SESIÓN
2 PATVIRTINTA NACIONALINĖS TEISMŲ ADMINISTRACIJOS DIREKTORIAUS 2014 M SAUSIO
OSNUTEK – ZA JAVNO OBRAVNAVO NA PODLAGI TRETJEGA ODSTAVKA
 PROTOCOLO DE TRATAMIENTO DEL CÁNCER DE PULMÓN METASTÁSICO EN
PROTOCOLO DE TRATAMIENTO DEL CÁNCER DE PULMÓN METASTÁSICO EN DECLARACIÓN DE CONFORMIDAD EL FABRICANTE O SU REPRESENTANTE LEGAL
DECLARACIÓN DE CONFORMIDAD EL FABRICANTE O SU REPRESENTANTE LEGAL ARQUIVO DO REINO DE GALICIA DÍA INTERNACIONAL DOS ARQUIVOS
ARQUIVO DO REINO DE GALICIA DÍA INTERNACIONAL DOS ARQUIVOSRESOURCE REQUEST (ICS 213 RR) ADAPTED FOR COVID 1