COPYRIGHT INFORMATION OF THE ARTICLE PUBLISHED ONLINE TITLE TWIN
COPYRIGHT (C) 19972006 BY43 © COPYRIGHT 2004 NORBERT MOCH KLEISTSTR
REBASE THE RESTRICTION ENZYME DATABASE HTTPREBASENEBCOM COPYRIGHT (C)
! COPYRIGHT (C) MICROSOFT CORPORATION ALL RIGHTS RESERVED
!doctype Html html Langen Classnojs ! Content Copyright National
(UPDATED DECEMBER 2003) COPYRIGHT NOTICE COPYRIGHT 1988 1991 1992
2005-04-25


Copyright Information of the Article Published Online
|
TITLE |
Twin pregnancy with triple parathyroid adenoma: A case report and review of literature |
|
AUTHOR(s) |
Yu Zhang, Jin-Wang Ding, Ling-Ying Yu, Ding-Cun Luo, Jian-Liang Sun, Zhi-Kai Lei, Zhi-Hua Wang |
|
CITATION |
Zhang Y, Ding JW, Yu LY, Luo DC, Sun JL, Lei ZK, Wang ZH. Twin pregnancy with triple parathyroid adenoma: A case report and review of literature. World J Clin Cases 2018; 6(11): 466-471 |
|
URL |
http://www.wjgnet.com/2307-8960/full/v6/i11/466.htm |
|
DOI |
http://dx.doi.org/10.12998/wjcc.v6.i11.466 |
|
OPEN ACCESS |
This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ |
|
CORE TIP |
Primary hyperparathyroidism (PHPT) during pregnancy is rare and has been previously reported, but a case of PHPT in a twin pregnancy with three parathyroid adenomas at the same time has not been reported. Multiple parathyroid lesions are difficult to diagnose, and pregnant women who insist upon continuing a pregnancy are not suitable to undergo 99mTc-sestamibi scintigraphy. These results in a case of PHPT that is easily misdiagnosed and can have serious consequences for the patient and the fetus. Therefore, we reviewed the difficulties encountered during the diagnosis and treatment of this case to improve the understanding of this disease and reduce the incidence of incorrect and missed diagnoses. |
|
KEY WORDS |
Primary hyperparathyroidism; Pregnancy; Triple parathyroid adenoma; Surgery |
|
COPYRIGHT |
© The Author(s) 2018. Published by Baishideng Publishing Group Inc. All rights reserved. |
|
NAME OF JOURNAL |
World Journal of Clinical Cases |
|
ISSN |
2307-8960 |
|
PUBLISHER |
Baishideng Publishing Group Inc, 7901 Stoneridge Drive, Suite 501, Pleasanton, CA 94588, USA |
|
WEBSITE |
Http://www.wjgnet.com |
CASE REPORT
Twin pregnancy with triple parathyroid adenoma: A case report and review of literature
Yu Zhang, Jin-Wang Ding, Ling-Ying Yu, Ding-Cun Luo, Jian-Liang Sun, Zhi-Kai Lei, Zhi-Hua Wang
Yu Zhang, Jin-Wang Ding, Ding-Cun Luo, Department of Oncology, Affiliated Hangzhou First People’s Hospital, Zhejiang University School of Medicine, Hangzhou 310006, Zhejiang Province, China
Ling-Ying Yu, Department of Endocrinology, Affiliated Hangzhou First People’s Hospital, Zhejiang University School of Medicine, Hangzhou 310006, Zhejiang Province, China
Jian-Liang Sun, Department of Anesthesiology, Affiliated Hangzhou First People’s Hospital, Zhejiang University School of Medicine, Hangzhou 310006, Zhejiang Province, China
Zhi-Kai Lei, Department of Ultrasound Branch, Affiliated Hangzhou First People’s Hospital, Zhejiang University School of Medicine, Hangzhou 310006, Zhejiang Province, China
Zhi-Hua Wang, Department of Obstetrics and Gynecology, Affiliated Hangzhou First People’s Hospital, Zhejiang University School of Medicine, Hangzhou 310006, Zhejiang Province, China
Author contributions: Luo DC was accountable for the execution of the case report and the integrity and analysis of the data; Ding JW, Lei ZK, Sun JL, Wang ZH and Yu LY collected patient’s clinical data; Zhang Y, Ding JW and Yu LY analyzed the data and wrote the paper; all authors read and approved the final manuscript.
Supported by the Key Project of Scientific and Technological Innovation in Hangzhou, NO. 20131813A08; the Key Project of Medical Scientific and Technology Program in Hangzhou, NO. 2013Z04; the Traditional Chinese Medical Science Research Program of Zhejiang Province, NO. 2018239534; the Applied Research Project of Commonweal Technology in Zhejiang Province, NO. 2017C33180.
Correspondence to: Ding-Cun Luo, MD, Chief Doctor, Professor, Surgeon, Department of Oncology, Affiliated Hangzhou First People’s Hospital, Zhejiang University School of Medicine, No. 261 Huansha Road, Hangzhou 310006, Zhejiang Province, China. [email protected]
Telephone: +86-571-56006981 Fax: +86-571-87914773
Received: June 21, 2018 Revised: July 20, 2018 Accepted: August 6, 2018
Published online: October 6, 2018
Abstract
Primary hyperparathyroidism (PHPT) is rare during pregnancy. A case of twin pregnancy with three simultaneous parathyroid adenomas at the same time has not been reported. Multiple parathyroid lesions are difficult to diagnose, as pregnant women who insist upon continuing a pregnancy are not able to undergo 99mTc-sestamibi scintigraphy, so cases of PHPT are easily unobserved and often can have serious consequences for the patient and the fetus. Therefore, we reported a case of a 28-year-old woman mid-pregnancy with twins, who had hypercalcemia and was eventually diagnosed with twin pregnancy with PHPT due to a triple parathyroid adenoma, had good pregnancy outcomes after undergoing surgery in mid-pregnancy. Twin pregnancy with PHPT due to a triple parathyroid adenoma, as presented in this case, is very rare and surgery in mid-pregnancy is demonstrated here as safe. Intraoperative parathormone monitoring was and remains key to a successful operation.
Key words: Primary hyperparathyroidism; Pregnancy; Triple parathyroid adenoma; Surgery
© The Author(s) 2018. Published by Baishideng Publishing Group Inc. All rights reserved.
Zhang Y, Ding JW, Yu LY, Luo DC, Sun JL, Lei ZK, Wang ZH. Twin pregnancy with triple parathyroid adenoma: A case report and review of literature. World J Clin Cases 2018; 6(11): 466-471 Available from: URL: http://www.wjgnet.com/2307-8960/full/v6/i11/466.htm DOI: http://dx.doi.org/10.12998/wjcc.v6.i11.466
Core tip: Primary hyperparathyroidism (PHPT) during pregnancy is rare and has been previously reported, but a case of PHPT in a twin pregnancy with three parathyroid adenomas at the same time has not been reported. Multiple parathyroid lesions are difficult to diagnose, and pregnant women who insist upon continuing a pregnancy are not suitable to undergo 99mTc-sestamibi scintigraphy. These results in a case of PHPT that is easily misdiagnosed and can have serious consequences for the patient and the fetus. Therefore, we reviewed the difficulties encountered during the diagnosis and treatment of this case to improve the understanding of this disease and reduce the incidence of incorrect and missed diagnoses.
INTRODUCTION
Primary hyperparathyroidism (PHPT) is a rare disease characterized by parathyroid glands that secrete excessive parathyroid hormone (PTH), which causes disorders associated with calcium and phosphorus levels and bone metabolism. Parathyroid adenoma is the most common cause of PHPT. The prevalence of PHPT is 1/4000 and is found more commonly in women. The ratio of cases in males compared to female cases is about 1:3[1]. According to the literature, 85%-90% of PHPTs are solitary, and less than 2% of patients have 2 or more leisons[2]. PHPT with pregnancy is rarer[3], and can be masked by normal pregnancy conditions, resulting in it being easily misdiagnosis or incorrectly diagnosed. A consensus has not yet been reached regarding a treatment plan, as more conservative treatments or a surgical treatment are both associated with great risks. Treatment that is not timely, it can have serious consequences for both the mother and the fetus. Treatment of multiple parathyroid adenomas in pregnancy is totally a tricky proposition. There are no reports in the literature on a twin pregnancy complicated by multiple parathyroid adenomas. Therefore, this is the first report of a the diagnosis and treatment of a case of twin pregnancy where the mother experienced PHPT due to a triple parathyroid adenoma that was admitted to our hospital in November 2017 is reported for the first time.
CASE REPORT
The patient was a first-time mother who was 28-year-old. Because of suffering from “endometriosis”, she has been trying to get pregnant for 2 years since she married, but she had not become pregnant due to ongoing endometriosis. She became pregnant through in-vitro fertilization and embryo transfer. At the 22nd week of pregnancy, she was admitted to the endocrinology department of our hospital on November 2, 2017, as she exhibited elevated serum levels of calcium for one month. The patient presented to the local hospital with severe vomiting, nausea, and general weakness at 18 wk of gestation. The obstetrical ultrasound showed a twin pregnancy, and a blood test showed that her blood potassium level was 1.5 mmol/L (normal range 3.5 to 5.30 mmol/L) and blood calcium level 2.79 mmol/L (normal range 2.00 to 2.60 mmol/L). Although symptoms were relieved after emergency rehydration and potassium supplementation, there is no immediate treatment for hypercalcemia. Therefore, it was found later that her blood potassium level had been corrected, but her blood calcium level gradually increased (3.47 mmol/L), so she was transferred to our hospital for further treatment. Physical examination: The patient’s spirit is soft, the skin and sclera were not yellow, the superficial lymph nodes were not swollen, the limbs were not deformed, the thyroid gland was not swollen, the heart and lungs were not remarkably affected, the lower abdomen was bulging, no tenderness and rebound tenderness were observed, no lower extremity edema was observed, and no negative neuropathological signs were observed. Past disease history: The patient had no history of long-term use of vitamins A, D, and calcium, and had no family history of specific diseases. Supplementary examination: PTH 187 pg/mL (normal range 15-65 pg/mL), serum calcium level was 3.49 mmol/L, serum phosphorus level was 0.62 mmol/L (normal range 0.8-1.5 mmol/L), and alkaline phosphatase level was 76 mmol/L (35-100 u/L). Ultrasound on her neck revealed a moderately echogenic nodule (2.0 cm × 0.8 cm) on the dorsal side of the superior portion of the left thyroid gland, which first suggested a parathyroid adenoma. A nodule was observed in the inferior dorsal lateral aspect of the right thyroid gland that was classified as a “3” on the TI-RADS evaluation scale. Admission diagnosis: twin pregnancy with PHPT that was possibly attributable to parathyroid adenomas. After admission, we performed fluid rehydration, diuresis, dilatation, and combined symptomatic supportive, such as calcitonin administration. Blood calcium and PTH levels decreased slightly but did not change much. After several discussions with the multiple-disciplinary team (MDT), and repeatedly communication with the patient, we told her about the advantages and disadvantages as they related to more conservative treatment options. Finally, the patient and her family chose surgical treatment.
After a fully preoperative preparation, resection of the parathyroid tumor was performed using a cervical plexus nerve block on November 16, 2017. During the operation, a tumor on the dorsal side of the superior lobe of the left thyroid was first observed (lesion 1), which was observed by ultrasound examination. No abnormal mass was found inferior lobe of the left thyroid. After resection of the above masses, blood PTH level was 131 pg/mL (preoperatively is 187 pg/mL) 10 min after resection, which failed to fall to an ideal value. Then, we began to explore the area behind the right thyroid lobe and found two more lesions: one in the superior dorsal lobe of the right thyroid (lesion 2) and one in the lateral aspect of the right lower lobe (lesion 3), with sizes of approximately 2.5 cm × 1.5 cm × 1.0 cm and 0.6 cm × 0.5 cm × 0.5 cm, respectively. Intraoperative puncture eluent results confirmed that the above lesions were parathyroid tissues, and the blood PTH level was 39 pg/mL 10 min after complete resection of the other two lesions (lesion 2 and 3), and freezing pathology also suggested that parathyroid adenoma should be first considered as the cause. To prevent postoperative hypocalcemia, relatively normal lesions (approximately 3 mm × 3 mm × 3 mm) were placed in the patient’s forearm muscles. Postoperative PTH and serum calcium were within the reference values. Postoperative pathology suggested that the positioning of the lesions at positions of “upper left, lower right, upper right” is consistent with parathyroid adenomas. In follow-up, we found that the patient had undergone a cesarean delivery for 1 male and 1 female infant at 32 wk of gestation, and the newborns were basically normal for preterm infants except for the general performance in that they exhibited low weight. Blood calcium and PTH levels were normal during the follow-up of the patient and the infants.
DISCUSSION
Pregnancy with PHPT is rare[4]. There are only 150 cases of related diseases reported in the literature, and less than 10 cases reported in China. This is the first case of PHPT in a twin pregnancy with multiple parathyroid tumors. PHPT can lead to serious complications for both the mother and fetus[5]. Common complications for the mother include: hyperemesis, skeletal lesions, kidney stones, elevated blood pressure, and other similar complications. When serum calcium is extremely elevated, it can induce pancreatitis, and a high blood calcium crisis can lead to death. A total of 80% of patients who do not receive effective treatment will experience complications in the fetus that can include fetal growth restriction, low birth weight, premature birth, intrauterine fetal death, stillbirth and neonatal hand-foot convulsions. According to literature reports, the incidence of untreated maternal complications in PHPT is about 67% of all pregnancy-associated PHPT cases, and the incidence of fetal or neonatal complications is as high as 80%, and can cause fetal or neonatal death in as much as 30% of cases. Therefore, it is necessary to raise the awareness of the disease.
Most patients who experience PHPT while pregnant lack typical clinical manifestations. Clinical symptoms often only manifest as vomiting, polydipsia, increased nocturia, and other similar symptoms. These are easily to be confused with normal responses to pregnancy, thereby masking the condition and causing missed diagnoses. In this case, due to nausea, vomiting and general malaise were present, but subsequent examinations also revealed a progressive increase in serum levels of calcium, and parathyroid tumors were found after assessing PTH levels and were partly observed through ultrasound examination. Combined with other people’s reports and our experience in this case[6,7], when a pregnant woman presents with the following symptoms: Hyperemesis, spasticity, pancreatitis, hypercalcemia, urinary system stones, this disease should be considered. If blood calcium and PTH levels are observed over time and can be combined with ultrasound, 99mTc-sestamibi scintigraphy, then the diagnosis of the disease is not difficult, and suggesting that raised awareness of the disease is most important for its correct diagnosis. However, it should be emphasized that 99mTc-sestamibi scintigraphy should be avoided for those who elect to continue with a pregnancy because of their associated risks of radiation exposure, as shown as example demonstrates. Additionally, the disease needs to be differentiated from other diseases, such as hypercalcemia that could be caused from a multiple myeloma or other similar causes, and secondary hyperparathyroidism, familial hyperparathyroidism syndrome, diseases that affect multiple endocrine glands, and other additional possible causes of these symptoms. These can be identified by combining laboratory and imaging tests with an oral history.
Current PHPT treatment guidelines do not give a clear treatment plan in PHPT associated with pregnancy as the incidence of PHPT in pregnancy is very low and most of the literature only reports individual cases. Norman et al[8] analyzed 32 women who had PHPT while pregnant and found that about 20% of patients who received surgical treatment during the middle of pregnancy had a good outcomes associated with the pregnancy. When a PHPT patient remains untreated, loss of the pregnancy can occur in as many as 40% of untreated pregnancies. Therefore, it is considered that early diagnosis and active surgical treatment are necessary. However, some researchers[5] found through retrospective analysis that there was no statistically significant difference in the live birth rate compared to the rate of abortion in pregnancies associated with PHPT compared to normal pregnancies, and that only the cesarean section rate increased slightly. Therefore, parathyroid surgery should be considered, as PHPT does not reduce the risk of miscarriage in these patients, but surgery can still help reduce the complications in both the mother and the newborn. However, risks associated with surgery are also very high, including risks associated with anesthesia, postoperative bleeding, permanent hypoparathyroidism, and other similar complications. Any risk may have serious consequences for the mother, the child, or both. In addition, more conservative treatment may be considered for patients with PHPT who exhibit only mildly elevated serum calcium levels in PHPT, as studies suggesting that patients with asymptomatic PHPT with serum calcium levels below 11 mg/dL (2.75 mmol/L) should consider more conservative treatments, which include treatments like administration of calcitonin, and other similar options[9]. At present, the conservative treatment methods for PTPH mainly include rehydratation, Calcitonin, Bisphosphonates and Cinacalcet. The use of rehydratation and Calcitonin is relatively mature, and no adverse effects of the fetus have been reported in the literature. Bisphosphonates and Cinacalcet can cross the placenta and are embryotoxic at high doses[10]. Although these have been used in few cases with good results, but more evidence of safety is required[11]. However, conservative treatments and their effects are often limited, and drug resistance may occur. If pregnant women with PHPT do not receive effective treatment, the incidence of neonatal complications can reach up to 80% of all cases of PHPT in pregnancy. Even in conservatively treated patients, the incidence of neonatal complications can reach as high as 53%, of which 27% to 31% of these cases can result in neonatal deaths[12]. In summary, current evidence supports parathyroidectomy as the main treatment, performed preferably during the second trimester, when the serum calcium is above 11 mg/dL (2.75 mmol/L). In the patients with mild forms of PHPT, which are nowadays the most frequent, a conservative management is generally preferred[13]. We think the timing of surgical management of PHPT in pregnancy also should also think over acute maternal presentation, fetal status, maternal medical and surgical history, and the patient’s response to medical management.
In this case, the patient’s blood calcium and PTH levels were decreased somewhat but remained elevated overall after medical treatment. If we had continued with a more conservative treatment, there would have likely been an escape phenomenon, which can lead to severe consequences, such as: Refractory hypercalcemia, possibly a high calcium crisis, hematuria, coma, and death. Current research has confirmed that surgery performed during the second trimester of pregnancy is largely safe, but surgery performed in later stages of pregnancy can increase miscarriage rates. Our patient was in the second trimester, so it was the best time for surgery for this patient. Therefore, after a multidisciplinary discussion in the hospital, and repeatedly stressing advantages and disadvantages of each treatment option to the patient and her family, the patient chose surgery. Although most reports say that general anesthesia has little effect on the mother and the fetus, we still chose a nerve block in the cervical plexus to reduce possible harm to the mother and the fetus. Finally, in follow-up, we observed a good outcome relating to the pregnancy in this patient.
The surgical treatment of hyperparathyroidism is an organ-destructive surgery. Its success requires not only a return of normal PTH levels, but also an avoidance of overcorrection and prevention of permanent hypoparathyroidism. Multiple parathyroid lesions are more problematic in clinical treatment. The literature shows that 85%-90% of PHPT are solitary, and less than 2% of patients have 2 or more lesions[2]. Precise preoperative imaging to obtain the lesion’s location is beneficial for a rapid search for parathyroid lesions, and it is also especially helpful for improving the success rate of the surgery, as it can reduce the time of the surgery and exposure to anesthesia, which is especially important for this patient. Ultrasound examination is a convenient, inexpensive and non-invasive examination method. The accuracy of preoperative localization of parathyroid lesions alone can be up to reach 77% (173/226)[14], which is comparable to the accuracy of a radionuclide scan plus MIBI imaging alone. The latter can be used when the ultrasound examination is negative or uncertain. The combination of these two examinations can increase the accuracy of positioning to 90%. Ultrasound, 99mTc-sestamibi scintigraphy, and MRI have their own advantages and disadvantages in PHPT diagnosis. Reasonable selection can complement each other. However, the literature reports and our experience in this case suggest that any imaging examination cannot ensure the visualization of all paraneoplastic lesions in these glands. More importantly, visualization of lesions depends on the surgeon’s experience and careful exploration during surgery, especially in patients like the one in this case who was not able to undergo 99mTc-sestamibi scintigraphy. In addition, the immediate detection of changes in PTH levels during surgery is also an important measure for improving the success of the surgery[15]. PTH is metabolized by the liver and kidneys in vivo. Its half-life is only 3 to 5 min. High serum PTH reduction is the earliest change indicating success in surgical treatment of PHPT. The standard that is currently most widely accepted by the majority of scholars is the Miami standard: The surgery is considered successful if the value of the PTH serum level drops to greater than or equal to 50% of the preoperative PTH value 10 min after the gland is removed. Therefore, being able to observe changes in PTH serum levels at 10 min after the surgical removal of the gland is critical for assessing the success of the operation. This case uses this criterion. After resection of the patient’s supra-parathyroid tumor prompted by preoperative ultrasound, PTH levels in the blood (131 pg/mL) did not drop to the expected level, so we continued to explore the right neck and found two additional lesions. The intraoperative puncture of eluent results suggested that the two masses originated in the parathyroid gland. After the second complete resection of the two lesions, the levels of PTH in the blood dropped to 39 pg/mL, suggested the surgery had completely removed all parathyroid lesions.
To avoid overcorrection and prevent the occurrence of permanent hypoparathyroidism, we chose a relatively normal lesion of about 3 mm × 3 mm × 3 mm in size for autologous transplantation in the forearm muscles in this patient, which was done according to the guidelines developed from the experiences from the treatment of patients with secondary hyperparathyroidism. After postoperative follow-up, blood PTH and serum calcium levels in this patient were within the normal range. However, in the case of similar patients, the need for transplantation of the parathyroid glands and the amount of transplanted tissue necessary must be further explored and studied. Additionally, the literature reports that about 5% of patients have ectopic parathyroid lesions. If this patient is involved in this situation, what should we do? PTH levels may remain substandard after all suspected lesions have been removed, but if the surgeon continues to probe blindly, it undoubtedly will increase the surgical complications and even possibly cause increased serious consequences. Recommendations for these cases require further research and lessons learned.
In summary, the possibility of PHPT should be considered during pregnancy when hypercalcemia, stones in the urinary tract, pancreatitis, prolonged irritability of pregnancy, or bone fractures occuring. Combined with experience of treatment in this patient, mid-pregnancy surgery has been previously observed as relatively safe. Early diagnosis and treatment of PHPT during pregnancy can result in better pregnancy outcomes. In addition, failure to perform surgery for PHPT surgery may result in a secondary surgery or permanent hypoparathyroidism, which may cause great pain to patients. In clinical practice, a rigorous diagnosis and treatment strategy must be established. Our experience suggests that imaging cannot be fully relied upon for diagnosis. The rapid detection of PTH levels using a process called intraoperative parathormone monitoring (IPM) after surgical resection is necessary and key for a successful operation, and the removal of diseased glands should return PTH levels to their ideal value. The treatment plan should allow for individual choices based on the patient’s symptoms, serum calcium levels, the effectiveness of more conservative treatments, the size of the gestational age in the patient and the patient’s willingness to receive the chosen treatment.
ARTICLE HIGHLIGHTS
Case characteristics
The patient presented with nausea, vomiting and general malaise and elevated serum calcium.
Clinical diagnosis
Physical examination showed the patient’s spirit is soft, the lower abdomen is bulging.
Differential diagnosis
The differential diagnosis included multiple myeloma, secondary hyperpaathyroidism, familial hyperparathyroidism syndrome and multiple endocrine gland diseases. The disease can be differentiated from other diseases by asking history and combining laboratory, imaging tests.
Laboratory diagnosis
Blood test results were as follows: Parathyroid hormone (PTH) 187 pg/mL, serum calcium 3.49 mmol/L, serum phosphorus 0.62 mmol/L, alkaline phosphatase 76 mmol/L.
Imaging diagnosis
Ultrasound on the neck showed a moderately echogenic nodule (2.0 cm × 0.8 cm) on the dorsal side of the upper left thyroid gland, which parathyroid adenoma was the first consideration. Thyroid right lower lobe dorsal lateral process nodule (TI-RADS 3).
Pathological diagnosis
Postoperative pathology suggested that “three lesions are all parathyroid adenomas”.
Treatment
Treatment with parathyroid tumor resection the cervical plexus nerve block during mid-pregnancy.
Related reports
Primary hyperparathyroidism during pregnancy have been reported previously, they were all have a single parathyroid adenoma or choose to complete the radiological examination after termination of pregnancy. But we report a unique case of twin pregnancy with three parathyroid adenomas, without radiological examination, had good pregnancy outcomes after undergoing surgery during mid-pregnancy.
Term explanation
IPM: Intraoperative parathormone monitoring.
Experiences and lessons
Given the severity of the associated complications, every effort should be made to ensure prompt diagnosis and reasonable treatment. Do not rely on imaging diagnosis. Careful exploration, rapid detection of PTH after surgical resection and the removal of diseased glands to the ideal value, which called IPM is the key to successful operation.
REFERENCES
1 Yeh MW, Ituarte PH, Zhou HC, Nishimoto S, Liu IL, Harari A, Haigh PI, Adams AL. Incidence and prevalence of primary hyperparathyroidism in a racially mixed population. J Clin Endocrinol Metab 2013; 98: 1122-1129 [PMID: 23418315 DOI: 10.1210/jc.2012-4022]
2 Amaya García M, Acosta Feria M, Soto Moreno A, Dios Fuentes E, Navarro González E, Quijada Thong D, Del Valle A, Acosta Delgado D, Astorga Jiménez R. Primary hyperparathyroidism in pregnancy. Gynecol Endocrinol 2004; 19: 111-114 [PMID: 15624273 DOI: 10.1080/09513590400002334]
3 Hirsch D, Kopel V, Nadler V, Levy S, Toledano Y, Tsvetov G. Pregnancy outcomes in women with primary hyperparathyroidism. J Clin Endocrinol Metab 2015; 100: 2115-2122 [PMID: 25751112 DOI: 10.1210/jc.2015-1110]
4 Rchachi M, El Ouahabi H, Boujraf S, Ajdi F. Primary hyperparathyroidism in pregnancy. Ann Afr Med 2017; 16: 145-147 [PMID: 28671157 DOI: 10.4103/aam.aam_61_16]
5 Abood A, Vestergaard P. Pregnancy outcomes in women with primary hyperparathyroidism. Eur J Endocrinol 2014; 171: 69-76 [PMID: 24743398 DOI: 10.1530/EJE-13-0966]
6 Kamenický P, Lecoq AL, Chanson P. Primary hyperparathyroidism in pregnancy. Ann Endocrinol (Paris) 2016; 77: 169-171 [PMID: 27157105 DOI: 10.1016/j.ando.2016.04.010]
7 Zeng H, Li Z, Zhang X, Wang N, Tian Y, Wang J. Anesthetic management of primary hyperparathyroidism during pregnancy: A case report. Medicine (Baltimore) 2017; 96: e9390 [PMID: 29390544 DOI: 10.1097/MD.0000000000009390]
8 Norman J, Politz D, Politz L. Hyperparathyroidism during pregnancy and the effect of rising calcium on pregnancy loss: a call for earlier intervention. Clin Endocrinol (Oxf) 2009; 71: 104-109 [PMID: 19138316 DOI: 10.1111/j.1365-2265.2008.03495.x]
9 Som M, Stroup JS. Primary hyperparathyroidism and pregnancy. Proc (Bayl Univ Med Cent) 2011; 24: 220-223 [PMID: 21738295 DOI: 10.1080/08998280.2011.11928719]
10 Djokanovic N, Klieger-Grossmann C, Koren G. Does treatment with bisphosphonates endanger the human pregnancy? J Obstet Gynaecol Can 2008; 30: 1146-1148 [PMID: 19175968 DOI: 10.1016/S1701-2163(16)34026-9]
11 Edling KL, Korenman SG, Janzen C, Sohsman MY, Apple SK, Bhuta S, Yeh MW. A pregnant dilemma: primary hyperparathyroidism due to parathyromatosis in pregnancy. Endocr Pract 2014; 20: e14-e17 [PMID: 24013984 DOI: 10.4158/EP13105.CR]
12 Schnatz PF, Curry SL. Primary hyperparathyroidism in pregnancy: evidence-based management. Obstet Gynecol Surv 2002; 57: 365-376 [PMID: 12140371 DOI: 10.1097/00006254-200206000-00022]
13 Dochez V, Ducarme G. Primary hyperparathyroidism during pregnancy. Arch Gynecol Obstet 2015; 291: 259-263 [PMID: 25367603 DOI: 10.1007/s00404-014-3526-8]
14 Solorzano CC, Carneiro-Pla DM, Irvin GL 3rd. Surgeon-performed ultrasonography as the initial and only localizing study in sporadic primary hyperparathyroidism. J Am Coll Surg 2006; 202: 18-24 [PMID: 16377493 DOI: 10.1016/j.jamcollsurg.2005.08.014]
15 Bian XH, Li SJ, Zhou L, Zhang CH, Zhang G, Fu YT, Sun H. Applicability of rapid intraoperative parathyroid hormone assay through fine needle aspiration to identify parathyroid tissue in thyroid surgery. Exp Ther Med 2016; 12: 4072-4076 [PMID: 28105137 DOI: 10.3892/etm.2016.3896]
Footnotes
Informed consent statement: Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Conflict-of-interest statement: The authors declare that they have no conflicts of interest.
CARE Checklist (2013) statement: The authors have read the CARE Checklist statement, and the manuscript was prepared and revised according to the CARE Checklist statement.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Peer-review started: June 21, 2018
First decision: July 8, 2018
Article in press: August 6, 2018
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Li B, Rong G S- Editor: Ji FF L- Editor: A E- Editor: Song H
01524 0203 (R 0506) THE UNIVERSITY OF VERMONT COPYRIGHT
12 MUSIC PROGRAM FOR HP28S HP48XX CALCULATOR COPYRIGHT ©
18 IKEMUCOPYRIGHT KOD INVENTORI KEPINTARAN EMOSI MALAYSIA – UNIVERSITI
Tags: article published, 2018 article, copyright, title, information, online, published, article
- ANALISIS COMPARATIVO DE PROPIEDADES FISICOQUIMICAS DE COMPOSITES DENTALES FOTOPOLIMERIZADOS
- BÖLÜM 9 SIRALAMA (SORTING) 91 GIRIŞ SIRALAMA VE
- RESULTADOS FASE ZONAL SUR 1432013 IES GRIÑÓN IES RESULTADOS
- 1 BILAG 6 – HVORDAN SKAL DETTE UDFYLDES KORREKT?
- RESPUESTA DE LOS ABUELOS A ANMAR® AGRADECEMOS ALTAMENTE ESE
- ZESTAW GIER I ZABAW 1 „ SADZENIE ZIEMNIAKÓW” PRZYBORY
- ZLINEU ZÁKLADNÍ INFORMACE POVINNĚ ZVEŘEJŇOVANÉ INFORMACE
- CÉSAR VALDEOLMILLOS ALONSO ¿NEGOCIAR? ¿PARA QUÉ? ¿NEGOCIAR? ¿PARA QUÉ?
- STATUTORY DECLARATION OATHS ACT 1900 (NSW)1 I [INSERT FULL
- A YUNTAMIENTO DE AJOFRIN (TOLEDO) CONCEJALÍA DE CULTURA NORMAS
- TOUR DE COMBIN IN MOUNTAIN BIKE RACCONTO E IMPRESSIONI
- FAKTA OM ADHD DET ER SVÆRT VIKTIG AT HELSEINFORMASJON
- REGIONŲ KREPŠINIO LYGOS 20192020 M 20202021 M ČEMPIONATŲ NUOSTATAI
- RESOLUTION OF THE MEMBERS OF [FULL LEGAL NAME
- ZAJEDNICA ŠPORTA DUBROVAČKONERETVANSKE ŽUPANIJE PRIJAVA PROGRAMA ZA ZADOVOLJENJE JAVNIH
- ZAHTJEV ZA IZMJENE I DOPUNE REGISTRACIJEBRISANJA IZ REGISTRA UDRUGAZAKLADA
- COMMONWEALTH OF MASSACHUSETTS APPELLATE TAX BOARD ROCKRIDGE LAKE SHORES
- GRANSKNING AV MILJÖSTYRNING I PROJEKT INNEHÅLLSFÖRTECKNING FÖRORD 1 SAMMANFATTNING
- BRIEFING NOTES STANDING COMMITTEE ON FISHERIES AND OCEANS RE
- ADDITIONS TO AGENDA 924TH REGULAR MEETING OF COUNCIL
- JUNTA DE ANDALUCIA CONSEJERÍA DE AGRICULTURA PESCA Y DESARROLLO
- PROFESSIONAL AND CLINICAL STANDARDS CONTACT SUSAN DOUTHWAITE DIRECT TEL
- NOMOR ISTIMEWA BANDUNG …………… LAMPIRAN 1 (SATU)
- CVIČENÍ 2 – PRÁCE SE SOUBORY VYTVOŘTE NA
- WHY DID HENRY DISSOLVE THE MONASTERIES? IN 1535 THERE
- POESÍA “ LA JIRAFA” LA JIRAFA SE PASEA CON
- 8 NISAN 2009 ÇARŞAMBA RESMÎ GAZETE SAYI 27194
- ………………………… Dnia ………………… (miejscowość) ……………………………………… ……………………………………… ……………………………………… (dane Kontaktowe
- MĚSTO ČESKÝ KRUMLOV NÁM SVORNOSTI 1 IČO 245836 BANKSPOJENÍ
- AKSARA FONT TIPOGRAFI BASKORO SURYO BANINDRO DISAJIKAN DALAM RANGKA
KLAUZULA INFORMACYJNA DOTYCZĄCA PRZETWARZANIA DANYCH OSOBOWYCH WŁAŚCICIELI OD KTÓRYCH
 1021 MOHSEN ABDELTAWWAB ET AL USE OF SPIRULINA (ARTHROSPIR
1021 MOHSEN ABDELTAWWAB ET AL USE OF SPIRULINA (ARTHROSPIRECONOMÍA II MICROECONOMÍA PRÁCTICA 2 1 SUPONGA QUE
 BALDINTZA CARATULA DE PLIEGO DE ADMINISTRATIBO CLAUSULAS BEREZIEN ORRIAREN
BALDINTZA CARATULA DE PLIEGO DE ADMINISTRATIBO CLAUSULAS BEREZIEN ORRIAREN BANCO DE PALABRAS Y ORACIONES PROGRAMA DE LECTOESCRITURA EVA
BANCO DE PALABRAS Y ORACIONES PROGRAMA DE LECTOESCRITURA EVA MODELO GENERICO DE MANIFESTACION RESPONSABLE DE VIGENCIA REPRESENTANTE LEGAL
MODELO GENERICO DE MANIFESTACION RESPONSABLE DE VIGENCIA REPRESENTANTE LEGAL İŞYERİ EĞİTİMİ ESASLARI VE TARAFLARIN YÜKÜMLÜLÜKLERİNE İLİŞKİN SÖZLEŞME
İŞYERİ EĞİTİMİ ESASLARI VE TARAFLARIN YÜKÜMLÜLÜKLERİNE İLİŞKİN SÖZLEŞME  SOMMARIO PER RIDURRE DRASTICAMENTE LE PERDITE OCCULTE MALE ENDEMICO
SOMMARIO PER RIDURRE DRASTICAMENTE LE PERDITE OCCULTE MALE ENDEMICO STYREINSTRUKS FOR AS ORGANISASJONSNUMMER XXXXXXXXX FØLGENDE INSTRUKS GJELDER FOR
STYREINSTRUKS FOR AS ORGANISASJONSNUMMER XXXXXXXXX FØLGENDE INSTRUKS GJELDER FOR TEMA 3 PIAŢA COMPONENTĂ ESENŢIALĂ A MEDIULUI DE MARKETING
TEMA 3 PIAŢA COMPONENTĂ ESENŢIALĂ A MEDIULUI DE MARKETING YANZHOU COAL MINING COMPANY LIMITED THE STOCK EXCHANGE OF
YANZHOU COAL MINING COMPANY LIMITED THE STOCK EXCHANGE OFCOMPTE RENDU DÉTAILLÉ DE L’OBSERVATOIRE NATIONAL SUR LA NOTION
DTOP SNE CAPÍTULO IV DE LA LEY LEY Nº
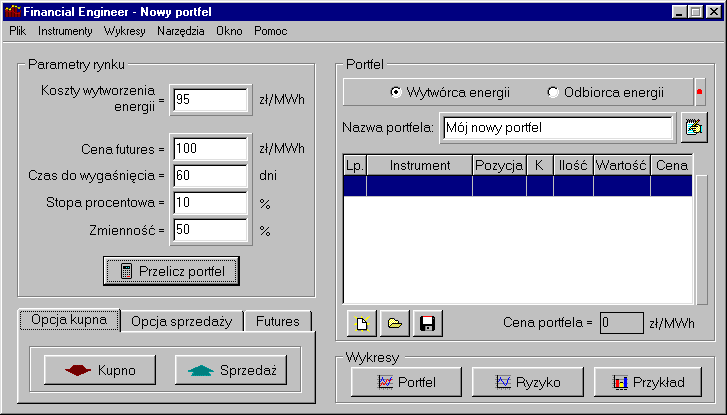 COPYRIGHT (C) 1999 WERON FINANCIAL ZARZĄDZANIE RYZYKIEM NA RYNKU
COPYRIGHT (C) 1999 WERON FINANCIAL ZARZĄDZANIE RYZYKIEM NA RYNKU Nº ACTA CONSEJO SECTORIAL DE CULTURA FECHA 30112010 HORA
Nº ACTA CONSEJO SECTORIAL DE CULTURA FECHA 30112010 HORA (DOMANDA DI AMMISSIONE SU CARTA INTESTATA DELL’AZIENDA) SPETTLE CONSIGLIO
(DOMANDA DI AMMISSIONE SU CARTA INTESTATA DELL’AZIENDA) SPETTLE CONSIGLIOCURRICULUM VITAE INFORMACIÓN PERSONAL NOMBRE LUIS ALFREDO BLOCH PINO
 XV OLIMPIADA PROVINCIAL DE MATEMÁTICAS PARA ALUMNOS DE 1º
XV OLIMPIADA PROVINCIAL DE MATEMÁTICAS PARA ALUMNOS DE 1ºZARZĄDZENIE NR 771 IX 2020 BURMISTRZA GOŁDAPI Z
OKRESNÍ SOUD VE FRÝDKUMÍSTKU NA POŘÍČÍ 3206 738 13