SEIZURE SCENARIO AN 11YEAROLD MALE IS TRANSFERRED FROM A
BARBARA CHMIELEWSKA KRZYSZTOF TUROWSKI MIGRAINETRIGGERING EPILEPTIC SEIZURES MIGRALEPSYHOW BEST TO RECORD SEIZURES KEEPING A RECORD OF
INTERNATIONAL NARCOTICS CONTROL BOARD NOTIFICATION ON SEIZURES OF INTERNATIONALLY
SEIZURE LIST 1 DATE TIME & PLACE SEIZURE
SEIZURE SCENARIO AN 11YEAROLD MALE IS TRANSFERRED FROM A
ST JOHNS COUNTY SCHOOL DISTRICT MEDICAL MANAGEMENT PLAN SEIZURE
Seizure Scenario
An 11-year-old male is transferred from a local community hospital to the Pediatric Trauma Emergency Department for treatment following a head injury. He was playing football and collided head first with another player. He had a loss of consciousness (LOC) for 2 minutes after the incident. Initial CT scan at the sending facility was negative for intracranial bleeding. Patient continues to ask repetitive questions and is amnesic to the event. CT scan of neck was also negative and patient denies neck or back pain. The report received was that the pupils are PERRL at 3mm and patient has no deficits other than the memory loss. The patient has a history of diabetes, has no known allergies to medicine, and has an implanted insulin pump. The patient weighs 45kg. Following the patient’s arrival to the unit as a report is being given by the transport team, the patient begins to have a generalized or tonic-clonic seizure.
General code outline
Nurse proceeds to the bedside and assesses the patient. Patient is having generalized tonic clonic seizure activity, is unresponsive and has snoring respirations.
Staff initiates the rapid response team/code team (facility dependent). Staff performs ABCs and applies 100% O2 via non-rebreather (NRB) mask. Gather resuscitation equipment. Seizure precautions are put in place to protect patient from harm. Patient is placed on cardiac, blood pressure and pulse-ox monitors.
Transport team informs the nurse of patient’s diabetic history. PIV has already been established by the transport team. The patient’s blood glucose level is checked and is 45. Rapid response team begins to administer dextrose (dose appropriate for weight) but the IV is nonfunctional. Attempt another IV placement if accessible. Otherwise, IO placement is necessary.
IO placement established and dextrose is given.
Reassess ABCs and blood glucose level. Seizure activity continues unchanged after administering glucose. Repeat glucose is 185. Patient is having snoring respirations and generalized seizure activity. Staff are unable to read the pulse-ox due to seizure activity.
ABCs continue to be monitored. Orders for medication to stop seizure activity are received, prepared and administered by staff.
Patient’s seizure activity slows down but continues. Staff should prepare another dose of medication to stop seizure activity as ordered by attending physician.
Patient’s seizure activity has ceased. Patient is unresponsive and has snoring respirations. Patient’s airway suctioned and repositioned. SpO2 91% on 100% NRB. Patient’s gag reflex intact. A nasal pharyngeal airway (NPA) is placed.
Reassess and monitor ABCs. Continue with complete exam. Evaluate studies done at sending facility. Consider repeating CT scan to detect change in status. Consult neurology.
Skills reviewed:
ABCs including airway maintenance including NPA use and suction equipment
General assessment
Knowledge of location of resuscitation equipment
Knowledge of use of rapid response teams
Proper dosage and preparation of medications
Reassessment after procedures
Knowledge of recommended resuscitation guidelines
Knowledge of altered mental status, diabetic and seizure precaution treatment protocols
|
Event/Assessment |
Action Required |
|
Patient is having generalized tonic clonic seizure activity, is unresponsive and has snoring respirations. |
Nurse will initiate the rapid response team/code team (facility dependent). Perform assessment of ABCs and applies 100% O2 via non-breather mask. Gather resuscitation equipment. Initiate seizure precautions to protect patient from harm. Place patient on cardiac, blood pressure and pulse-ox monitors. |
|
Transport team informs the nurse of patient’s diabetic history. PIV has already been established by the transport team. |
Blood glucose level is checked due to history of diabetes. |
|
Blood glucose is 45. |
Rapid response team begins to administer dextrose but the IV is nonfunctional. Participants should calculate dosage and prepare medication. Attempt another IV placement if accessible. Otherwise, IO placement is necessary. |
|
IO placement established and dextrose is given. |
Reassess patient and glucose level. ABCs continue to be monitored. |
|
Seizure activity continues unchanged after administering glucose. Repeat glucose is 185. Unable to read pulse-ox due to seizure activity. Patient continues to have snoring respirations and generalized seizure activity. |
Orders for medication to stop seizure activity are ordered (as per facility protocol), prepared and administered. Participants should calculate dosage and prepare medication. |
|
Patient’s seizure activity slows down but continues |
Second order for medication to stop seizure activity given by physician. Participants should calculate dosage and prepare medication. |
|
Patient’s seizure activity has ceased. Patient is unresponsive and has snoring respirations. SpO2 91% on 100% NRB. Patient’s gag reflex intact. |
Patient’s airway suctioned and repositioned. Patient’s gag reflex is tested and is present. NPA placed. |
|
Patient’s SpO2 at 96% with NPA in place. Patient’s ABCs maintained. |
Reassess and monitor ABCs. Continue with complete exam. Evaluate studies done at sending facility. Consider repeat CT scan to detect changes. Consult neurology. |
Tags: seizure, scenario, 11yearold, transferred
- AVOIN YLIOPISTO TIETOJENKÄSITTELYOPIN PERUSTEET PORTFOLIO JUKKA SALMINEN AVOIN
- EL SERVICIO NACIONAL DE ADUANAS HA PUESTO A DISPOSICIÓN
- 0 IFIF 17 DICEMBRE 2021 UFFICIO CCORRIERE DEL TICINO
- UNIVERSITY OF NORTH CAROLINA AT WILMINGTON DEPARTMENT OF MUSIC
- MINISTERIO SECRETARÍA GENERAL DE LA PRESIDENCIA COMISIÓN NACIONAL DEL
- FAKULTETA ZA ELEKTROTEHNIKO KATEDRA ZA ELEKTROENERGETSKE SISTEME IN NAPRAVE
- 1 NAPISATI PROGRAM SA FUNKCIJOM ZA IZRAČUNAVANJE SUME KVADRATA
- LA ESCUELA DEMOCRÁTICA UN CAMBIO PARA LOS CIUDADANOS D
- MINIT CURAI MESYUARAT PEMANTAPAN PENGENDALIAN PENGURUSAN PBS PERINGKAT NEGERI
- LIST IF INVITEES TO THE CONVERGENCE THINK TANK SEMINAR
- TRIBUNALE ORDINARIO DI ROVIGO AFFARI CIVILI NON CONTENZIOSI DA
- FREDERIKSHAVN PARTIFORENING STANDARDVEDTÆGTER FOR FORENINGER § 1 FORENINGENS
- ESPACIO [RE]ACTIVADO DANIEL JIMÉNEZ FERRERA ARQUITECTO LA CASA SACERDOTAL
- REGIONÁLIS KÖZÖSSÉGI KÖZPONTOK TEDD JOBBÁ! 2020 PROGRAM KÖZBENSŐ BESZÁMOLÓJÁNAK
- MINISTERIO DE HACIENDA LEY NÚM 20460 (PUBLICADA EN EL
- P WWWGRIPAHR ISMO PACIJENTU GRIPA JE OZBILJNA BOLEST KOJA
- MINISTERO DELL’ISTRUZIONE DELL’UNIVERSITÀ E DELLA RICERCA PUBBLICAZIONE AI SENSI
- EL ESQUELETO HUMANO 1005AA SISTEMA ESQUELETICO LA INCREÍBLE FLEXIBILIDAD
- LINEAMIENTOS PARA LA SOLICITUD DE APOYO FINANCIERO PARCIAL PARA
- OZNACZENIE SPRAWY PN0311W SPECYFIKACJA ISTOTNYCH WARUNKÓW ZAMÓWIENIA NA SKŁAD
- ZAŁĄCZNIK NR 2 FORMULARZ OFERTY DOWOLNY KSZTAŁT KSZTAŁT 1
- RECRUITMENT MONITORING FORM NAME…………………………………… POST APPLIED FOR ……………………………………… NORFOLK
- S AFETY AND HEALTH SERVICES FIRST AID SUPPLIES ORDER
- 5 CONVENCIONES (¿?) NO ES CLARO EL CONTENIDO POR
- METAMORPHIC ROCK CLASSIFICATION AND IDENTIFICATION LAB MRS COHN EARTH
- PLENARIO 154 LEY Nº 8040 8040 NORMAS DEL PRESUPUESTO
- LIBROS Y REGISTROS QUE DEBEN LLEVAR LAS PERSONAS FÍSICAS
- P RINTED OCTOBER 5 2021 PLAN ORGÁNICO DE PRODUCCIÓN
- PROPERTY INSURANCE NEW LOCATION QUESTIONNAIRE (TO BE COMPLETED BY
- TECHNICAL NOTE MESSAGING INFRASTRUCTURE SUPPORT FOR VALIDATION
LUTKOVNA PREDSTAVA EMILY HORNČRNI MUC PRIREDILA BREDA VARL GLASBENA
[IME I PREZIME AUTORA] OIB TEL
CONTACT AHN HYUNHO DIRECTOR INDUSTRIAL TECHNOLOGY POLICY DIVISION (21105171)
MATH 260 – LINEAR ALGEBRA SYLLABUS FOR SECTION 0C1
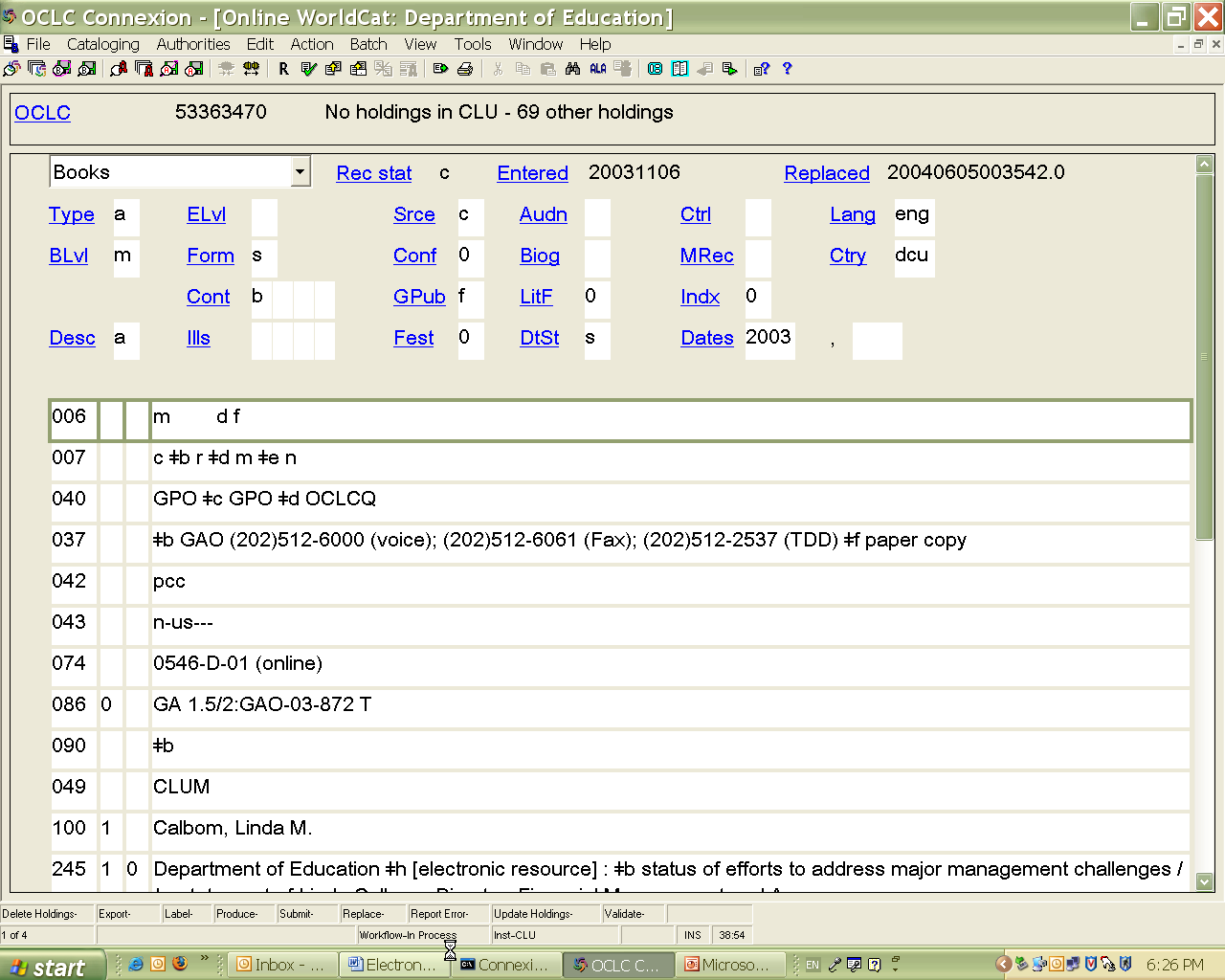 CATALOGING EBOOKS 71207 REV CPK FIXED FIELDS 1 WORKFORM
CATALOGING EBOOKS 71207 REV CPK FIXED FIELDS 1 WORKFORMZARZĄDZENIE REKTORA UNIWERSYTETU EKONOMICZNEGO W KRAKOWIE NR R0201192018 Z
[WSL132] CONSIDER ADDING CSS GRID FALLBACK (USING FLEXBOX) FOR
 OOH CARE PATHWAYS PATIENT’S JOURNEY HOME NHS
OOH CARE PATHWAYS PATIENT’S JOURNEY HOME NHSPOČET ABSOLVENTŮ V DSP PODLE JEDNOTLIVÝCH OBORŮ V R
REFERENCES TO APPENDICES AAGAARD K COACHMAN LK AND CARMACK
SIGORTA ŞIRKETI HASARTAZMINAT PERSONELI (SEVIYE 5) 13UMS03005 13022013
 KEMENTERIAN PENDIDIKAN DAN KEBUDAYAAN UNIVERSITAS NEGERI SEMARANG GEDUNG
KEMENTERIAN PENDIDIKAN DAN KEBUDAYAAN UNIVERSITAS NEGERI SEMARANG GEDUNG EXPOSÉ GOUVERNANCE RENAULT NISSAN INTRODUCTION NOUS SOMMES
EXPOSÉ GOUVERNANCE RENAULT NISSAN INTRODUCTION NOUS SOMMES TO NEGOTIATE SUCCESSFULLY THE INITIAL PLANNING AND RESEARCH WORK
TO NEGOTIATE SUCCESSFULLY THE INITIAL PLANNING AND RESEARCH WORK RESS612 ANNEX 4B ISOLATION RESISTANCE MEASUREMENT METHOD FOR COMPONENT
RESS612 ANNEX 4B ISOLATION RESISTANCE MEASUREMENT METHOD FOR COMPONENT KODAS 123944821 SALTONIŠKIŲ G 58 LT08105 VILNIUS TEL FAKS
KODAS 123944821 SALTONIŠKIŲ G 58 LT08105 VILNIUS TEL FAKS LINKSTM SUMMER 2014 LITERACY PROGRAM A GREAT WAY TO
LINKSTM SUMMER 2014 LITERACY PROGRAM A GREAT WAY TO CÂMARA MUNICIPAL DE CORDISBURGO RUA GOVERNADOR VALADARES 16 –
CÂMARA MUNICIPAL DE CORDISBURGO RUA GOVERNADOR VALADARES 16 – KURS „HISTORISCHE GRUNDBEGRIFFE“ SCHLOTHEUBER VIII KAISER KÖNIG KÖNIGSWÄHLER 7
KURS „HISTORISCHE GRUNDBEGRIFFE“ SCHLOTHEUBER VIII KAISER KÖNIG KÖNIGSWÄHLER 7CSO1225A (316) ARIZONA DEPARTMENT OF CHILD SAFETY OFFICE OF