INTRACORONARY ACETYLCHOLINE PROVOCATION IN PATIENTS WITH UNOBSTRUCTED CORONARY ARTERIES
INTRACORONARY ACETYLCHOLINE PROVOCATION IN PATIENTS WITH UNOBSTRUCTED CORONARY ARTERIES
Coronary Artery Spasm As A Frequent Cause Of Acute Coronary Syndrome –
Intracoronary acetylcholine provocation in patients with unobstructed coronary arteries
Clinical Usefulness, Angiographic Characteristics and Safety Evaluation of Intracoronary Acetylcholine Provocation Testing Among 921 Consecutive
Caucasian Patients with Unobstructed Coronary Arteries
Peter Ong, MD1; Anastasios Athanasiadis, MD1; Gabor Borgulya, MD,MSc2; Ismail Vokshi3; Rachel Bastiaenen, MBBS3, Sebastian Kubik3, Stephan Hill, MD1, Tim Schäufele, MD1, Heiko Mahrholdt, MD1, Juan Carlos Kaski MD,DSc3, and Udo Sechtem, MD1
1 Robert-Bosch-Krankenhaus, Department of Cardiology, Auerbachstr. 110, 70376 Stuttgart, Germany.
2 St George’s University of London, Clinical Trials Unit, London, United Kingdom
3 Cardiovascular Sciences Research Centre, St George’s University of London, London, United Kingdom
Address for correspondence:
Peter Ong, M.D., Robert-Bosch-Krankenhaus, Department of Cardiology, Auerbachstr. 110, 70376 Stuttgart, Germany; Phone: +49-711-81016048; Fax: +49-711-81013795, E-Mail: [email protected]
Word count: 4417
Abbreviations:
ACH = acetylcholine
CAD = coronary artery disease
ECG = electrocardiogram
LCA = left coronary artery
RCA = right coronary artery
Abstract and keywords
Background: Coronary spasm can cause myocardial ischemia and angina in patients with and those without obstructive coronary artery disease. However, provocation tests using intracoronary acetylcholine administration (ACH-test) are rarely performed in clinical routine in the US and Europe. Thus, we assessed the clinical usefulness, angiographic characteristics and safety of the ACH-test in Caucasian patients with unobstructed coronaries.
Methods and results: From September 2007-June 2010, a total of 921 consecutive patients (362 men, mean age 62±12years) who underwent diagnostic angiography for suspected myocardial ischemia and were found to have unobstructed coronaries (no stenosis ≥50%) were enrolled. The ACH-test was performed directly after angiography according to a standardized protocol. Three-hundred-forty-six patients (35%) complained chest pain at rest, 222 (22%) chest pain upon exertion, 238 (24%) a combination of effort and resting chest pain and 41 (4%) presented with troponin positive acute coronary syndrome. The overall frequency of epicardial spasm (>75% diameter reduction with angina and ischemic ECG-shifts) was 33.4% and of microvascular spasm (angina and ischemic ECG-shifts without epicardial spasm) 24.2%. Epicardial spasm was most often diffuse and located in the distal coronary segments (p<0.01). No fatal or irreversible non-fatal complications occurred. However, 9 patients (1%) had minor complications [non-sustained ventricular tachycardia (n=1), fast paroxysmal atrial fibrillation (n=1), symptomatic bradycardia (n=6), catheter-induced spasm (n=1)].
Conclusions: Epicardial and microvascular spasm are frequently found in Caucasians with unobstructed coronaries. Epicardial spasm is most often diffuse and located in the distal coronary segments. The ACH-test is a safe technique to assess coronary vasomotor function.
Keywords: acetylcholine, coronary spasm, microvascular spasm, complications.
Introduction
Since its inaugural description in 1959 (1), coronary artery spasm has been recognized as an important cardiac condition that can lead to myocardial ischemia and angina pectoris in patients with as well as those without obstructive coronary artery disease (2). Coronary spasm can be the cause for myocardial infarction (3) and ventricular arrhythmias (4) and it has been shown that coronary spasm can also occur on the level of the microcirculation (5). It has been suggested that coronary spasm is more prevalent among Asian as compared to Caucasian populations (6,7) and that Caucasians more often have focal coronary spasm associated with an atherosclerotic plaque rather than diffuse spasm in the distal parts of the epicardial vessels (8). Moreover, it has been hypothesized that the frequency of coronary spasm is on the decrease in the Western world (9). However, provocation testing using intracoronary acetylcholine administration in search of coronary spasm is rarely performed in daily clinical routine in the US and Europe. In this study, we sought to assess the frequency of epicardial and microvascular coronary spasm, the angiographic characteristics and the safety of intracoronary acetylcholine provocation testing (ACH-test) in a contemporary cohort of 921 consecutive Caucasian patients with unobstructed coronary arteries.
Methods
Patients
From September 2007 to June 2010, a total of 921 consecutive patients (362 men, mean age 62±12years) who underwent diagnostic coronary angiography for suspected myocardial ischemia and were found to have unobstructed coronary arteries (no epicardial stenosis ≥50%) were included in the study. Intracoronary acetylcholine provocation testing was performed directly after diagnostic coronary angiography. Subjects were excluded and the provocation test was not performed if patients had severe chronic obstructive pulmonary disease or impaired renal function (creatinine >2.0 mg/dl), or if spontaneous spasm was observed. The following information was recorded in every patient: Clinical presentation (chest pain at rest, chest pain upon exertion, a combination of both, or other symptoms); previous history of obstructive coronary artery disease including previous coronary stent implantation or coronary artery bypass surgery (CABG); cardiovascular risk factors including hypertension, diabetes, hypercholesterolemia, a history of smoking and a positive family history for cardiovascular events (myocardial infarction or stroke in a parent or sibling); presentation with troponin positive acute coronary syndrome (STEMI or NSTEMI); results of non-invasive stress tests for myocardial ischemia (a positive response was defined as transient ischemic ECG changes ≥0.1mV in at least 2 continuous leads, 80ms after the J point and/or reproduction of angina during the stress test). Furthermore, the degree of narrowing along the epicardial vessels was quantified and categorized (0-20% and 21-49% narrowings). Patients with a previous history of obstructive coronary artery disease had all undergone revascularisation and were eligible because repeated coronary angiography due to recurrent symptoms and the suspicion of progress of CAD did not reveal any relevant epicardial stenosis.
Study protocol
The study protocol complied with the Declaration of Helsinki and all patients gave written informed consent before angiography. All patients in the study underwent intracoronary provocation with acetylcholine in accordance to a standardized protocol (10,11) immediately after diagnostic angiography. Cardiovascular medications (beta blockers, calcium channel blockers and nitrates) were discontinued 48 hours before coronary angiography. Sublingual glyceryltrinitrate administration was permitted for the relief of chest pain at all times. However, none of the patients required this treatment < 4 hours prior to angiography. Heart rate, blood pressure and the 12-lead-electrocardiogram were continuously monitored during ACH-testing. Ischemic ECG-changes were defined as transient ST-segment depression or elevation ≥0.1mV in at least two contiguous leads.
ACH Testing
Incremental doses of 2µg, 20µg, 100µg and 200µg of ACH were manually infused over a period of 3 minutes into the LCA via the angiographic catheter. In patients who remained asymptomatic and showed no diagnostic ST segment changes during LCA ACH infusion, 80µg of ACH were injected into the RCA (12). The ACH doses used in our protocol were derived from the multicentre ENCORE study (13). In this trial, the dose for the LAD and for the LCX was 100µg in each vessel injected via a selective catheter. For practical reasons the ACH-injection in the present study was performed unselectively via the diagnostic catheter in the LCA with a maximum dose of 200µg.
Transient AV-block was frequently observed, mostly during provocation of the RCA. It almost always resolved within seconds after reducing the speed of the manual injection. Therefore, we did not test the RCA with a pacing catheter in the right ventricle avoiding potential complications. A bolus of glyceryltrinitrate 0.2 mg (Perlinganit, Schwarz Pharma, Monheim, Germany) was injected into the LCA or RCA to relieve angina and/or severe epicardial constriction. Nitrates were also infused routinely at the end of the ACH-test into the RCA and LCA.
ACH Test Assessment
Angiographic responses during the ACH-test were analysed using computerized quantitative coronary angiography (QCA-CMS, Version 6.0, Medis-Software, Leiden, The Netherlands). The ACH-test was considered ‘positive’ for epicardial coronary spasm in the presence of focal or diffuse epicardial coronary diameter reduction ≥75% compared to the relaxed state following intracoronary nitroglycerine infusion in any epicardial coronary artery segment together with the reproduction of the patient’s symptoms and ischemic ECG shifts. Both the location and type of epicardial coronary spasm (i.e. focal vs. diffuse) were also assessed (14). ‘Focal’ constriction was defined as a circumscribed transient vessel narrowing within the borders of one isolated or two neighbouring coronary segments as defined by the American Heart Association (AHA). ‘Diffuse’ constriction was diagnosed when the vessel narrowing was observed in ≥ two adjacent coronary segments. Proximal spasm was defined as vasoconstriction occurring in segments 1, 5, 6 or 11. Mid-vessel spasm was recorded when occurring in segments 2, 3, 7, whereas distal spasm was defined as that occurring in segments 4, 8, 9, 10, 12, 13, 14 or 15.
‘Microvascular spasm’ was diagnosed when typical ischemic ST-segment changes and angina developed in the absence of epicardial coronary constriction ≥75% diameter reduction (5). Patients who experienced no angina, constriction or ST-segment shifts were considered to have a ‘negative’ ACH-test response (normal coronary vasoreactivity). The ACH-test was judged inconclusive in patients who only experienced angina without ECG changes. The same was true for those who had ST-segment shifts without reproduction of their symptoms. Finally, tests with angiographic vasospasm and ST-segment shifts but no angina were also defined to be inconclusive.
Statistical analysis
Data analysis was carried out using SPSS 17.0 (SPSS Inc., Chicago, Illinois, USA). Results are expressed as mean ± standard deviation. The t-test was used to compare continuous variables. The Fisher exact test was used for categorical variables. Multiple logistic regression analysis was performed using forward variable selection based on likelihood ratios to identify predictors for a pathologic ACH-test and for identification of patients with epicardial compared to those with microvascular spasm. A two-tailed p value of <0.05 was considered significant.
Results
Overall results
The summary of the results of all patients is shown in Table 1. In 74 of the 921 patients the ACH-test could not be performed due to logistic reasons or patient refusal. Among the remaining 847 patients the acetylcholine test revealed epicardial coronary spasm in 283 patients (33.4%) and microvascular spasm was seen in another 205 (24.2%) (Figure 1 and Figure 2). In 117 patients the ACH test was negative (no symptoms, no ECG changes, no epicardial spasm). In the remaining 242 patients the test was inconclusive as patients had reproduction of symptoms (n=87 ), ischemic ECG changes (n=81) and epicardial spasm (n=74, 40 with associated ischemic ECG changes but no reproduction of symptoms, one with reproduction of symptoms but without ECG shifts and 33 with neither of the latter) as the only abnormal finding, respectively.
Clinical characteristics
Overall, patients with a positive ACH test were older, more often female and they more often presented with exertional chest pain. In addition, they more often had a positive family history for cardiovascular disease and they more often showed a pathologic response to non-invasive stress testing. Interestingly, there were also fewer smokers in the group with an abnormal ACH-test compared to the group with a “negative” ACH-test.
Compared to patients with microvascular spasm, those with epicardial spasm were more often male and had a previous history of obstructive coronary artery disease. They more often presented with resting chest pain and a clinical presentation of ACS compared to the microvascular spasm group. The detailed results are shown in Table 2.
Multivariable analysis revealed that female gender, a previous history of coronary artery disease and a clinical presentation with effort angina or mixed angina were independent predictors for a pathologic ACH-test response (Table 3). Moreover, male gender, older age, cigarette smoking, a previous history of coronary artery disease, resting angina, lower left ventricular ejection fraction and a clinical presentation with acute coronary syndrome were identified as independent predictors for epicardial spasm compared to patients with microvascular spasm.
Angiographic characteristics of epicardial coronary spasm
Epicardial coronary spasm occurred in 378 vessels in 282 patients, including 190 (67%) with 1-vessel spasm, 88 (31%) with 2-vessel spasm, and 4 (1.4 %) with 3-vessel spasm. The most frequent type and location of spasm was distal and diffuse (40%, p<0.01, Figure 2 and Figure 3), mainly in segment 8 (distal LAD). Only 9 patients (3.2%) had a proximal and focal epicardial spasm. Patients with epicardial plaques between 21-49% had epicardial spasm more often (i.e. 45%) than patients with only minor coronary artery narrowings between 0-20% (i.e. 30%, p<0.01). However, spasm was found to be focally superimposed on insignificant atherosclerotic lesions in only 13 cases (4.6%).
Complications
We did not observe any fatal or serious non-fatal complications (e.g. sustained ventricular tachycardia, ventricular fibrillation or myocardial infarction due to prolonged coronary spasm). However, 9 patients (1%) suffered from minor complications. One patient developed non-sustained ventricular tachycardia during ACH-provocation and one had fast paroxysmal atrial fibrillation which resolved spontaneously after discontinuing the injection. Six patients developed symptomatic bradycardia and transient hypotension which resolved spontaneously after stopping the ACH injection in 5 - in one patient intravenous injection of atropine was necessary to stabilize heart rate and blood pressure. The remaining patient had catheter induced coronary spasm of the proximal right coronary artery associated with ST-segment elevation which resolved after removing the catheter. Apart from that, no other catheter induced spasms were observed. Statistical comparison of patients with and those without a complication did not reveal any significant differences (data not shown).
Discussion
This is the largest study to assess the safety of intracoronary acetylcholine provocation testing in Caucasian patients showing that the ACH-test is a safe method for the assessment of coronary vasomotor function when performed with an appropriate protocol. Moreover, we report a high frequency of coronary microvascular spasm in a large contemporary cohort of Caucasian patients with anginal symptoms and unobstructed coronary arteries. In addition, we could show that epicardial coronary spasm is most often diffuse and located in the distal parts of the epicardial vessels, probably as a sign of concomitant microvascular disease.
Clinical characterization
Comparison of clinical characteristics between patients with and those without coronary spasm revealed that female gender, a previous history of coronary artery disease and a clinical presentation with effort angina or mixed angina were independent predictors for a pathologic ACH-test response. In contrast to expectations, resting angina, male gender and cigarette smoking were not identified as significant predictors for the entire group. However, these variables were identified as predictors for epicardial spasm.
Our study extends previous data in so far that we also found a previous history of coronary artery disease, a lower left ventricular ejection fraction and a clinical presentation with acute coronary syndrome as independent predictors for the observation of epicardial spasm in response to acetylcholine testing. Therefore the results of our study provide a comprehensive clinical characterization of Caucasian patients with angina despite unobstructed coronary arteries with a high likelihood for epicardial spasm.
Microvascular spasm was also found to be frequent in our patients. Interestingly, hypertension and diabetes were not found to be predictors of microvascular spasm although both conditions are well known to impair microvascular function. However, diabetes was rather infrequent in our cohort and our data show that microvascular disease is also common in patients without a history of hypertension indicating that the feature “hypertension” has a good sensitivity (i.e. 80%) but does not have a high positive predictive value (i.e. 70%) for the presence of acetylcholine-induced coronary spasm. Moreover, all cardiovascular risk factors may have substantial and deleterious effects on the microcirculation as recently reported by Granger et al. (15).The fact that epicardial spasm was often distal and diffuse suggests that patients with microvascular spasm may also suffer from distal epicardial spasm as previously shown in smaller cohorts (16,17).Larger studies are needed to elucidate the relationship between epicardial and microvascular coronary vasomotor disorders.
Angiographic characteristics
The detailed analysis of the angiographic characteristics of our patients revealed that diffuse and distal epicardial coronary spasm was the most frequent finding. Our results contrast with a report in Caucasian patients by Bertrand et al. (6) who found most often focal epicardial spasm in their patients. This difference is most probably due to the different substance used for provocation of spasm (i.e. ergonovine in the study of Bertrand) and the different route of administration (intravenous vs. intracoronary). A study by Goto et al. showed that coronary spasm can often be elicited by acetylcholine even if ergonovine did not reveal any spasm (18). Moreover, our results are comparable with a more recent study by Coma-Canella et al. (19) suggesting that distal and diffuse spasm is a frequent observation in Caucasians with angina and unobstructed coronary arteries. In addition, the prevalence of coronary spasm of 32.3% reported in an Asian cohort of 685 Japanese patients appears to be similar to our findings (7).
Recently, Sato et al. (20) reported their findings from 1877 patients who underwent ACH-testing using similar criteria as in our study. They found a pathologic ACH-test response in 53% with 511 patients having focal spasm and 362 with diffuse spasm. Diffuse spasm was associated with a better prognosis after 5 years compared to focal spasm. In both studies, a positive family history for cardiovascular disease was more often found in patients with a spastic ACH-test response, albeit in our study with a higher frequency (i.e. 55.5% compared to only 17% in the Sato et al. study). Complication rates were similarly low in both studies. The main difference compared to our study is the inclusion of patients with an epicardial stenosis >75%. This probably explains the high number of patients with focal spasm (i.e. 59% of all patients with spasm) as compared to only 18% in our study. This is supported by a study from Okumura et al. (21) showing that diffuse spasm is frequently found in patients without advanced organic stenotic lesions. In addition, Saito et al. (22) showed that the presence of epicardial plaque is likely to be related to the occurrence of focal spasm. It should, however, be noted that there is currently no consensus definition for diffuse or focal coronary spasm. Clearly, comparative studies between Asian and Caucasian patients with stringent inclusion criteria and similar provocation test protocols should be performed to ultimately answer the question whether there are differences in prevalence and type of coronary spasm in ethnically diverse groups.
Safety
Due to its invasive nature, there has been a lot of scepticism regarding intracoronary provocation testing for coronary spasm because of the potential complications associated with the test. Interestingly, it is not the fact that coronary angiography is required for performing the test which raises concern but the fear of irreversible spasm leading to arrhythmia and death due to the provocative testing itself (9). However, previous studies in Asian as well as Caucasian patients have demonstrated that the test is reasonably safe. Bertrand et al. using intravenous ergonovine had no serious irreversible complications among their 1088 patients (6) and Harding et al. (23) reporting some 3447 intracoronary ergonovine tests in American patients only had a single patient with serious complications such as myocardial infarction or ventricular tachycardia/fibrillation corresponding to a complication rate of 0.03%. A higher complication rate was reported by Sueda et al., who used intracoronary acetylcholine in 685 patients and experienced sustained ventricular tachycardia, shock or cardiac tamponade in 1.3% of patients (7). In addition, Wei et al. (24) have recently reported their experience with 293 U.S. patients who underwent coronary reactivity testing reporting a complication rate of 0.7% for serious adverse events such as coronary artery dissection (one patient) and myocardial infarction (one patient). These complication rates are comparable with our rate of 1%. Thus, there is compelling evidence that the ACH-test using a stepwise approach with increasing doses as reported in our study is a safe procedure that can routinely be performed in the catheterization laboratory. One has to view these complication rates in context with current complication rates for diagnostic coronary angiography which are similar to those reported for acetylcholine testing (25, 26).
Clinical implications
The detection of abnormal coronary vasomotion in patients with anginal symptoms but angiographically unobstructed coronary arteries not only leads to reassurance of the patient that a cause for the symptoms is found but also enables the physician to initiate appropriate medical therapy (i.e. calcium channel blockers and nitrates (27)) aiming at reducing morbidity and mortality (28, 29). This may also have important implications on health care systems as most health care related costs in patients with unobstructed coronary arteries are due to recurrent or ongoing angina pectoris (30). Moreover, despite treatment with calcium channel blockers, patients with coronary spasm may suffer from persistent or recurrent episodes of angina at follow-up (31) underpinning the need for the development of new drugs for treatment of vasospastic angina. This report should also encourage interventionalists to add the ACH-test to their portfolio in search of functional causes for angina in patients with unobstructed coronary arteries (32). In patients presenting with symptoms other than angina pectoris (e.g. syncope or heart failure) ACH-testing may also be useful as these conditions can also be caused by coronary spasm (33, 34).
Limitations
Due to the fact that we did not challenge the RCA when coronary spasm was provoked in the LCA, the frequency of multivessel spasm may be underestimated.
We used a slightly different definition for epicardial coronary spasm than other investigators, especially from Asia (35) (i.e. ≥75% compared to subtotal vasoconstriction and a maximum dose of 200µg compared to 100µg acetylcholine as in the Asian protocols). Thus, the frequency of coronary spasm may be higher than with use of other definitions.
The acetylcholine test was not performed in the early morning in all patients. As a circadian variation of coronary spasm (36) has been described, the frequency of spasm might have been higher, if early morning exams had been conducted consistently.
Conclusions
Epicardial and microvascular coronary spasm are frequently found in Caucasian patients with anginal symptoms and unobstructed coronary arteries. Epicardial spasm is most often diffuse and located in the distal parts of the epicardial vessels. The ACH-test is a safe technique to assess coronary vasomotor function.
Acknowledgements
The authors are grateful to nurses and technicians in the catheterization laboratories and to all staff members of the Department of Cardiology, Robert-Bosch-Krankenhaus, Stuttgart, Germany for their help and support during the study.
Table 1: Patient characteristics – all patients
|
|
All patients |
ACH ‘pathologic’ |
ACH ‘negative’ |
p |
|
n= |
847 |
488 (58%) |
359 (42%) |
|
|
Sex (male, %) |
362 (43%) |
164 (34%) |
198 (55%) |
<0.0005 |
|
Age (mean±SD) |
61.8±11.6 |
62.8±11.1 |
60.5±12.1 |
0.006 |
|
Previous history of obstructive coronary artery disease |
164 (19%) |
105 (22%) |
59 (16%) |
0.065 |
|
Admissions for chest pain before ACH-test |
242 (28.6%) |
136 (28%) |
106 (29.5%) |
0.64 |
|
Diagnostic angiography before ACH-test |
274 (32.3%) |
167 (34%) |
107 (29.8%) |
0.18 |
|
Non-invasive test for ischemia performed (%) |
565 (66.7%) |
340 (70%) |
225 (62.7%) |
0.039 |
|
Positive response to non-invasive test for ischemia (%) |
328 (38.7%) |
210 (43%) |
118 (32.9%) |
0.023 |
|
Clinical presentation |
|
|
|
|
|
Predominantly resting chest pain |
346 (41%) |
168 (34%) |
178 (50%) |
<0.0005 |
|
Predominantly exertional chest pain |
222 (26%) |
145 (30%) |
77 (21%) |
0.007 |
|
Effort and resting chest pain |
238 (28%) |
154 (32%) |
84 (23%) |
0.011 |
|
Troponin positive ACS |
41 (5%) |
21 (4%) |
20 (6%) |
0.421 |
|
|
|
|
|
|
|
ACH-test |
|
|
|
|
|
LCA only |
556 (65.6%) |
395 (81%) |
161 (45%) |
<0.0005 |
|
RCA only |
2 (0.02%) |
1 (0.2%) |
1 (0.3%) |
1.0 |
|
LCA+RCA |
289 (34%) |
92 (19%) |
197 (55%) |
<0.0005 |
|
LVEF % (mean±SD) |
72±11 |
72±10 |
71±11 |
0.31 |
|
Risk factors: |
|
|
|
|
|
Hypertension |
609 (72%) |
346 (71%) |
263 (73%) |
0.49 |
|
Diabetes mellitus |
142 (17%) |
84 (17.2%) |
58 (16%) |
0.71 |
|
Hypercholesterolemia |
460 (54%) |
275 (56.3%) |
185 (52%) |
0.19 |
|
Smoking |
307 (36%) |
161 (33%) |
146 (41%) |
0.025 |
|
Positive family history for CVD |
441 (52%) |
271 (55.5%) |
170 (47.4%) |
0.022 |
ACS = acute coronary syndrome, CVD = cardiovascular disease, LCA = left coronary artery, LVEF = left ventricular ejection fraction, RCA = right coronary artery, SD = standard deviation.
Table 2: Patient characteristics according to ACH-test result
|
|
Epicardial spasm |
Microvascular spasm |
ACH-test inconclusive |
ACH-test ‘normal’ |
p-value* |
|
n= |
283 (33.4%) |
205 (24.2%) |
242 (28.6%) |
117 (13.8%) |
|
|
Sex (male, %) |
128 (45%) |
36 (18%) |
123 (51%) |
75 (64%) |
<0.0005 |
|
Age (mean±SD) |
63±11 |
62±11 |
61±12 |
60±12 |
0.025 |
|
Previous history of obstructive coronary artery disease |
79 (28%) |
26 (13%) |
45 (19%) |
14 (12%) |
<0.0005 |
|
Admissions for chest pain before ACH-test |
86 (30%) |
50 (24%) |
73 (30%) |
33 (28%) |
0.469 |
|
Diagnostic angiography before ACH-test |
105 (37%) |
62 (30%) |
75 (31%) |
32 (27%) |
0.188 |
|
Non-invasive test for ischaemia performed (%) |
193 (68%) |
147 (72%) |
155 (64%) |
70 (60%) |
0.119 |
|
Positive response to non-invasive test for ischemia (%) |
118 (42%) |
92 (45%) |
84 (35%) |
34 (29%) |
0.103 |
|
Clinical presentation |
|
|
|
|
|
|
Predominantly resting chest pain |
112 (40%) |
56 (27%) |
111 (46%) |
67 (57%) |
<0.0005 |
|
Predominantly exertional chest pain |
72 (25%) |
73 (36%) |
55 (23%) |
22 (19%) |
0.003 |
|
Effort and resting chest pain |
82 (29%) |
72 (35%) |
62 (26%) |
22 (19%) |
0.012 |
|
Troponin positive ACS |
17 (6%) |
4 (2%) |
14 (6%) |
6 (5%) |
0.128 |
|
|
|
|
|
|
|
|
ACH-test |
|
|
|
|
|
|
LCA only |
240 (84.8%) |
155 (76%) |
126 (52%) |
35 (30%) |
<0.0005 |
|
RCA only |
1 (0.4%) |
0 |
1 (0.3%) |
0 |
1.0 |
|
LCA+RCA |
42 (14.8%) |
50 (24%) |
115 (8%) |
82 (70%) |
<0.0005 |
|
LVEF % (mean±SD) |
71±11 |
74±10 |
71±11 |
72±11 |
0.010 |
|
Risk factors: |
|
|
|
|
|
|
Hypertension |
192 (68%) |
154 (75%) |
175 (72%) |
88 (75%) |
0.271 |
|
Diabetes mellitus |
50 (18%) |
34 (17%) |
41 (17%) |
17 (15%) |
0.912 |
|
Hypercholesterolemia |
167 (59%) |
108 (53%) |
121 (50%) |
64 (55%) |
0.207 |
|
Smoking |
113 (40%) |
48 (23%) |
108 (45%) |
38 (32%) |
<0.0005 |
|
Positive family history for CVD |
163 (58%) |
108 (53%) |
117 (48%) |
53 (45%) |
0.072 |
ACS = acute coronary syndrome, CVD = cardiovascular disease, LCA = left coronary artery, LVEF = left ventricular ejection fraction, RCA = right coronary artery, SD = standard deviation. * p refers to the comparison of all 4 patient groups.
Table 3: Multivariable analysis
|
Pathologic ACH-test vs. normal ACH-test |
Odds ratio, confidence interval, p-value |
|
Female gender |
2.501; 1.875 – 3.335; <0.0005 |
|
Previous history of coronary artery disease |
1.351; 1.058 – 1.552; 0.023 |
|
Clinical presentation without resting angina |
1.749; 1.314 – 2.330; <0.0005 |
|
Epicardial vs. microvascular spasm |
Odds ratio, confidence interval, p-value |
|
Male gender |
1.679; 1.491 – 1.798; <0.0005 |
|
Age |
1.023; 1.003 – 1.042; 0.022 |
|
Cigarette smoking |
1.463; 1.149 – 1.661; 0.008 |
|
Previous history of coronary artery disease |
1.536; 1.209 – 1.728; 0.005 |
|
Resting angina |
1.518; 1.261 – 1.685; 0.001 |
|
Clinical presentation with acute coronary syndrome |
1.749; 1.192 – 1.922; 0.020 |
|
Left ventricular ejection fraction |
0.979; 0.960 – 0.998; 0.034 |
Figure legend:
Figure 1: Study flow chart.
Figure 2: The upper panel shows LCA angiograms and ECGs of a patient with epicardial spasm. Note the diffuse but distally accentuated narrowing of the LAD during acetylcholine infusion (arrows) together with ischemic ECG shifts (A) and resolution of both findings after nitroglycerine i.c. (B). The lower panel shows an example of a patient with microvascular spasm. During ACH the patient had reproduction of angina, ischemic ECG changes but no epicardial constriction (C). After nitroglycerine i.c. chest pain and ECG changes resolved (D).
Figure 3: Graphic showing the distribution of type (diffuse, focal, combination) and location (proximal, mid-segment, distal, combination) of epicardial coronary artery spasm (n=283). The most frequent finding was a distal and diffuse spasm (40%, p<0.01).
Disclosures:
None
References:
1 Prinzmetal M, Kennamer R, Merliss R, Wada T, Bor N. Angina pectoris. I. A variant form of angina pectoris; preliminary report. Am J Med. 1959;27:375-88.
2 Cheng TO, Bashour T, Kelser GA Jr, Weiss L, Bacos J. Variant angina of Prinzmetal with normal coronary arteriograms. A variant of the variant. Circulation. 1973;47:476-85.
3 Maseri A, L'Abbate A, Baroldi G, Chierchia S, Marzilli M, Ballestra AM, Severi S, Parodi O, Biagini A, Distante A, Pesola A. Coronary vasospasm as a possible cause of myocardial infarction. A conclusion derived from the study of "preinfarction" angina. N Engl J Med. 1978;299:1271-7.
4 Myerburg RJ, Kessler KM, Mallon SM, Cox MM, deMarchena E, Interian A Jr, Castellanos A. Life-threatening ventricular arrhythmias in patients with silent myocardial ischemia due to coronary-artery spasm. N Engl J Med. 1992;326:1451-5.
5 Mohri M, Koyanagi M, Egashira K, Tagawa H, Ichiki T, Shimokawa H, Takeshita A. Angina pectoris caused by coronary microvascular spasm. Lancet. 1998;351:1165-9.
6 Bertrand ME, LaBlanche JM, Tilmant PY, Thieuleux FA, Delforge MR, Carre AG, Asseman P, Berzin B, Libersa C, Laurent JM. Frequency of provoked coronary arterial spasm in 1089 consecutive patients undergoing coronary arteriography. Circulation. 1982;65:1299-306.
7 Sueda S, Ochi N, Kawada H, Matsuda S, Hayashi Y, Tsuruoka T, Uraoka T. Frequency of provoked coronary vasospasm in patients undergoing coronary arteriography with spasm provocation test of acetylcholine. Am J Cardiol. 1999;83:1186-90.
8 Beltrame JF, Sasayama S, Maseri A. Racial heterogeneity in coronary artery vasomotor reactivity: differences between Japanese and Caucasian patients. J Am Coll Cardiol. 1999;33:1442-52.
9 Stern S, Bayes de Luna A. Coronary artery spasm: a 2009 update. Circulation. 2009;119:2531-4.
10 Ong P, Athanasiadis A, Hill S, Vogelsberg H, Voehringer M, Sechtem U. Coronary artery spasm as a frequent cause of acute coronary syndrome: The CASPAR (Coronary Artery Spasm in Patients With Acute Coronary Syndrome) Study. J Am Coll Cardiol. 2008;52:523-7.
11 Lüscher TF, Pieper M, Tendera M, Vrolix M, Rutsch W, van den Branden F, Gil R, Bischoff KO, Haude M, Fischer D, Meinertz T, Münzel T. A randomized placebo-controlled study on the effect of nifedipine on coronary endothelial function and plaque formation in patients with coronary artery disease: the ENCORE II study. Eur Heart J. 2009;30:1590-7.
12 Sueda S, Mineoi K, Kondo T, Yano K, Ochi T, Ochi N, Fukuda H, Kukita H, Kawada H, Matsuda S, Uraoka T. [Absence of induced spasm by intracoronary injection of 50 micrograms acetylcholine in the right coronary artery: usefulness of 80 micrograms of acetylcholine as a spasm provocation test]. J Cardiol. 1998;32:155-61.
13 ENCORE Investigators. Effect of nifedipine and cerivastatin on coronary endothelial function in patients with coronary artery disease: the ENCORE I Study (Evaluation of Nifedipine and Cerivastatin On Recovery of coronary Endothelial function). Circulation. 2003;107:422-8.
14 Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, Griffith LS, McGoon DC, Murphy ML, Roe BB. A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation. 1975;51(4 Suppl):5-40.
15 Granger DN, Rodrigues SF, Yildirim A, Senchenkova EY. Microvascular responses to cardiovascular risk factors. Microcirculation. 2010;17:192-205.
16 Sun H, Mohri M, Shimokawa H, Usui M, Urakami L, Takeshita A. Coronary microvascular spasm causes myocardial ischemia in patients with vasospastic angina. J Am Coll Cardiol. 2002;39:847-51.
17 Ong P, Athanasiadis A, Mahrholdt H, Borgulya G, Sechtem U, Kaski JC. Increased coronary vasoconstrictor response to acetylcholine in women with chest pain and normal coronary arteriograms (cardiac syndrome X). Clin Res Cardiol. 2012;101:673-81.
18 Goto A, Ito S, Kondo H, Nomura Y, Yasue N, Suzumura H, Takeda Y, Tomimoto S, Yamada Y, Horio T, Suzuki S, Fukutomi T, Itoh M. Evaluation of adjunctive intracoronary administration of acetylcholine following intravenous infusion of ergonovine to provoke coronary artery spasm. J Cardiol. 1999;34:309-16.
19 Coma-Canella I, Castano S, Macías A, Calabuig J, Artaiz M. Ergonovine test in angina with normal coronary arteries. Is it worth doing it? Int J Cardiol. 2006;107:200-6.
20 Sato K, Kaikita K, Nakayama N, Horio E, Yoshimura H, Ono T, Ohba K, Tsujita K, Kojima S, Tayama S, Hokimoto S, Matsui K, Sugiyama S, Yamabe H, Ogawa H. Coronary vasomotor response to intracoronary acetylcholine injection, clinical features, and long-term prognosis in 873 consecutive patients with coronary spasm: analysis of a single-center study over 20 years. J Am Heart Assoc. 2013;2:e000227.
21 Okumura K, Yasue H, Matsuyama K, Ogawa H, Kugiyama K, Ishizaka H, Sumida H, Fujii H, Matsunaga T, Tsunoda R. Diffuse disorder of coronary artery vasomotility in patients with coronary spastic angina. Hyperreactivity to the constrictor effects of acetylcholine and the dilator effects of nitroglycerin. J Am Coll Cardiol. 1996;27:45-52.
22 Saito S, Yamagishi M, Takayama T, Chiku M, Koyama J, Ito K, Higashikata T, Seguchi O, Honye J, Kanmatsuse K. Plaque morphology at coronary sites with focal spasm in variant angina: study using intravascular ultrasound. Circ J. 2003;67:1041-5.
23 Harding MB, Leithe ME, Mark DB, Nelson CL, Harrison JK, Hermiller JB, Davidson CJ, Pryor DB, Bashore TM. Ergonovine maleate testing during cardiac catheterization: a 10-year perspective in 3,447 patients without significant coronary artery disease or Prinzmetal's variant angina. J Am Coll Cardiol. 1992;20:107-11.
24 Wei J, Mehta PK, Johnson BD, Samuels B, Kar S, Anderson RD, Azarbal B, Petersen J, Sharaf B, Handberg E, Shufelt C, Kothawade K, Sopko G, Lerman A, Shaw L, Kelsey SF, Pepine CJ, Merz CN. Safety of coronary reactivity testing in women with no obstructive coronary artery disease: results from the NHLBI-sponsored WISE (Women's Ischemia Syndrome Evaluation) study. JACC Cardiovasc Interv. 2012;5:646-53.
25 Chandrasekar B, Doucet S, Bilodeau L, Crepeau J, deGuise P, Gregoire J, Gallo R, Cote G, Bonan R, Joyal M, Gosselin G, Tanguay JF, Dyrda I, Bois M, Pasternac A. Complications of cardiac catheterization in the current era: a single-center experience. Catheter Cardiovasc Interv. 2001;52:289-95.
26 Noto TJ Jr, Johnson LW, Krone R, Weaver WF, Clark DA, Kramer JR Jr, Vetrovec GW. Cardiac catheterization 1990: a report of the Registry of the Society for Cardiac Angiography and Interventions (SCA&I). Cathet Cardiovasc Diagn. 1991;24:75-83.
27 Yilmaz A, Sechtem U. Angina pectoris in patients with normal coronary angiograms: current pathophysiological concepts and therapeutic options. Heart. 2012;98:1020-9.
28 Johnson BD, Shaw LJ, Pepine CJ, Reis SE, Kelsey SF, Sopko G, Rogers WJ, Mankad S, Sharaf BL, Bittner V, Bairey Merz CN. Persistent chest pain predicts cardiovascular events in women without obstructive coronary artery disease: results from the NIH-NHLBI-sponsored Women's Ischaemia Syndrome Evaluation (WISE) study. Eur Heart J. 2006;27:1408-15.
29 Ong P, Athanasiadis A, Borgulya G, Voehringer M, Sechtem U. 3-year follow-up of patients with coronary artery spasm as cause of acute coronary syndrome: the CASPAR (coronary artery spasm in patients with acute coronary syndrome) study follow-up. J Am Coll Cardiol. 2011;57:147-52.
30 Shaw LJ, Merz CN, Pepine CJ, Reis SE, Bittner V, Kip KE, Kelsey SF, Olson M, Johnson BD, Mankad S, Sharaf BL, Rogers WJ, Pohost GM, Sopko G; Women's Ischemia Syndrome Evaluation (WISE) Investigators. The economic burden of angina in women with suspected ischemic heart disease: results from the National Institutes of Health--National Heart, Lung, and Blood Institute--sponsored Women's Ischemia Syndrome Evaluation. Circulation. 2006;114:894-904.
31 Bory M, Pierron F, Panagides D, Bonnet JL, Yvorra S, Desfossez L. Coronary artery spasm in patients with normal or near normal coronary arteries. Long-term follow-up of 277 patients. Eur Heart J. 1996;17:1015-21.
32 Ong P, Athanasiadis A, Sechtem U. Patterns of coronary vasomotor responses to intracoronary acetylcholine provocation. Heart. 2013, doi:10.1136/heartjnl-2012-302042.
33 Igarashi Y, Yamazoe M, Suzuki K, Tamura Y, Matsubara T, Tanabe Y, Yamaguchi T, Watanabe K, Aizawa Y, Shibata A. Possible role of coronary artery spasm in unexplained syncope. Am J Cardiol. 1990;65:713-7.
34 Inami T, Kataoka M, Shimura N, Ishiguro H, Kohshoh H, Taguchi H, Yanagisawa R, Hara Y, Satoh T, Yoshino H. Left ventricular dysfunction due to diffuse multiple vessel coronary artery spasm can be concealed in dilated cardiomyopathy. Eur J Heart Fail. 2012;14:1130-8.
35 JCS Joint Working Group. Guidelines for diagnosis and treatment of patients with vasospastic angina (coronary spastic angina) (JCS 2008): digest version. Circ J. 2010;74:1745-62.
36 El-Tamimi H, Mansour M, Pepine CJ, Wargovich TJ, Chen H. Circadian variation in coronary tone in patients with stable angina: Protective role of the endothelium. Circulation 1995;92:3201-5.
Tags: acetylcholine provocation, intracoronary acetylcholine, acetylcholine, patients, unobstructed, intracoronary, coronary, provocation, arteries
- APEL ZESPOŁU KEP DS APOSTOLSTWA TRZEŹWOŚCI I OSÓB UZALEŻNIONYCH
- U SUSRET OLIMPIJSKIM IGRAMA POSLJEDNJE PRIPREME U GOSPIĆU
- AUTOSHAPE 8 INSTRUCCIONES LA SIGUIENTE GUÍA TIENE POR OBJETIVO
- PILATES HOMEWORK NEUTRAL SPINE NEUTRAL SPINE IS A
- MODULE 11 GENERAL FOOD DISTRIBUTION PART 2 TECHNICAL NOTES
- DZIECI 3LETNIE GRUPA SMERFY WITAM RODZICE I DZIECI
- RALPH BARTON (BORN AUGUST 14 1891 KANSAS CITY MISSOURI
- AN ALLE BPMMITGLIEDER FEBRUAR 2018 BPMFACHEXKURSION NACH MYANMAR 2018
- PETITION TO APPROVE ALTERNATE HEALTH INSURANCE PLAN NAME PRINT
- SAĞLIK İÇİN ZEYTİNYAĞI BUGÜN DÜNYANIN EN ÖNEMLI KANSER ILACI
- GAGNGW42 PÁGINA 3 ORGANIZACIÓN MUNDIAL DEL COMERCIO GAGNGW42 5
- P L E A S E N O T
- 2021 HOUSE CAPTAINS CAPTAIN VICECAPTAIN WRIGHT AMARA S JONNY
- CONTENIDOS Y CRITERIOS DE EVALUACIÓN Y CALIFICACIÓN CURSOS4º ESO
- NZQA UNIT STANDARD 26184 VERSION 4 PAGE 5 OF
- FILE SYSTEM FILTER MANAGER FILTER DRIVER DEVELOPMENT GUIDE
- METODOLOGINIS PRANEŠIMAS DĖL 2020 M DUOMENŲ ATSKLEIDIMO 2021 METAIS
- MEMORANDUM OF UNDERSTANDING BETWEEN WARSAW UNIVERSITY OF TECHNOLOGY WARSAW
- EUROMOT POSITION GAS DRAFT COSTBENEFIT ASSESSMENT REPORTFINAL 20110915CORRDOC PAGE
- FACULTY COURSE PROPOSAL FORM – COURSE 1 PROFESSOR
- SILABUS MATA KULIAH DASAR BUSANA KODE MATA KULIAH
- EICMAR1 ROMUNSKI PROIZVAJALEC OBLAČIL IŠČE PARTNERJE ZA SKLENITEV LOHN
- GRIPPE SAISONNIÈRE ET INFECTIONS À PNEUMOCOQUE IMPRIMERENVOYER A
- JOSEP ROMA PICAS EMAIL JLLROMAYMAILCOM HISTORIA LABORAL TRABAJO
- KANDİLLİ BELEDİYE BAŞKANLIĞI KONU 2014 YILI FAALIYET RAPORU İMAR
- UDRUGA AUTSAJDER – NORI DVORI 2014 MULTIMEDIJSKI FESTIVAL NORI
- CONFLICT OF INTEREST IN RESEARCH FINANCIAL DISCLOSURE FORM COMPLETE
- FATTY ACIDS IN THE BLOOD REFLECT THE AMOUNT OF
- MAIL FROM TEUN BOKHOVEN 1410 DEAR JAN ERIK
- 1 INTRODUCCIÓN Y OBJETIVOS 1 QUÉ ES ANM (ASISTENCIA
SHARING TOYS I LIKE TO PLAY WITH TOYS WHEN
 EDUCATIONAL TALENT SEARCH ENHANCING EDUCATIONAL TALENT ENCOURAGING INDIVIDUAL SUCCESS
EDUCATIONAL TALENT SEARCH ENHANCING EDUCATIONAL TALENT ENCOURAGING INDIVIDUAL SUCCESS1 STANDART İSTİSNALAR SAĞLIK SIGORTASI GENEL ŞARTLARI MADDE2 VE
ELLEN FITZGERALD CONLY JANE LESLIE CRAZY LADY NY HARPERCOLLINS
4 KAUNO RAJONO KULTŪROS IR MENO PROJEKTŲ DALINIO FINANSAVIMO
ANNUAL PURCHASING DEADLINES APRIL 5 DEADLINE FOR REQUISITIONS UTILIZING
PELÍCULAS RECOMENDADAS PARA ESTOS DÍAS DE ENCIERRO 1 BRAVEHEART
UNITED NATIONS DEVELOPMENT PROGRAMME PROJECT OF THE GOVERNMENT OF
MUNICIPIO DE DOSQUEBRADAS (RISARALDA) CARACTERIZACIÓN GENERAL DEL ESCENARIOS DE
 E GROUP 6 XPERT OPINION GUIDELINE APPROVAL DATE 11
E GROUP 6 XPERT OPINION GUIDELINE APPROVAL DATE 112 DÍA DE LA CONCIENCIACIÓN DE LAS ENFERMEDADES INFLAMATORIAS
 INSTITUT FYZIKY VŠBTU OSTRAVA ZPRACOVAL NÁZEV PRÁCE MĚŘENÍ INTENZITY
INSTITUT FYZIKY VŠBTU OSTRAVA ZPRACOVAL NÁZEV PRÁCE MĚŘENÍ INTENZITY AAPD EMAILING LIST RENTAL ORDER FORM NAME COMPANY NAME
AAPD EMAILING LIST RENTAL ORDER FORM NAME COMPANY NAMEPARTICIPACIÓN CLUBES SLALOM OTOÑO 2006 PARTICIPACIÓN POR CATEGORÍAS EN
5 BETEGTÁJÉKOZTATÓ INFORMÁCIÓK A BETEG SZÁMÁRA CALCIUMSANDOZ PEZSGŐTABLETTA KALCIUM
 FORMATO DE APROBACIÓN MEDICAMENTOS POR FUERA DEL MANUAL ÚNICO
FORMATO DE APROBACIÓN MEDICAMENTOS POR FUERA DEL MANUAL ÚNICO MÉTODO FONÉTICO O FÓNICO SE CONSIDERA QUE FUE
MÉTODO FONÉTICO O FÓNICO SE CONSIDERA QUE FUEEMERGENCY PROCEDURES POST NEAR TELEPHONES AND AS APPROPRIATE IN
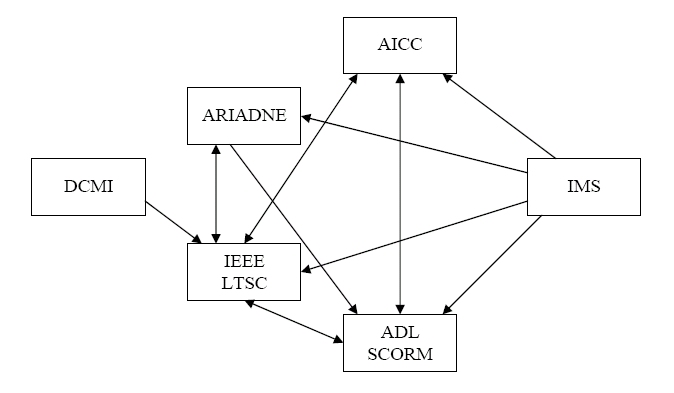 MEDIADORES E INTEROPERABILIDAD EN ELEARNING SANDRA AGUIRRE JUAN QUEMADA
MEDIADORES E INTEROPERABILIDAD EN ELEARNING SANDRA AGUIRRE JUAN QUEMADA FACULTAD DE INGENIERÍA EN ELECTRICIDAD Y COMPUTACIÓN FIEC
FACULTAD DE INGENIERÍA EN ELECTRICIDAD Y COMPUTACIÓN FIEC