DATE CONTINENCE ASSESSMENT CLINICAL HISTORY FEMALE
CONTINENCE PROBLEMS AFTER STROKE IT IS COMMON FOR PEOPLEDAILY HABITS AND URINARY INCONTINENCE EFFECTS OF DAILY MANY
DATE CONTINENCE ASSESSMENT CLINICAL HISTORY FEMALE
DISTRICT NURSING CONTINENCE ADVISORY SERVICE PHONE (03 684 1558
FORMULARY FOR INCONTINENCEMOISTURE SKIN PROTECTION GENERIC CATEGORY FUNCTION
GUIDANCE ON CONTINENCE AND INTIMATE CARE IN EARLY YEARS
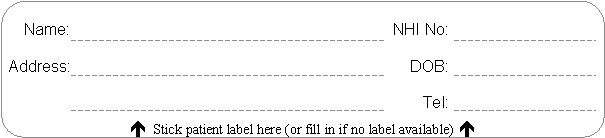
Urogynaecology Clinical History Form
![]()
Date: ______/______/______
Continence Assessment Clinical History - Female
Presenting complaint(s) and duration:
__________________________________________________________________________________________
__________________________________________________________________________________________
__________________________________________________________________________________________
__________________________________________________________________________________________
__________________________________________________________________________________________
__________________________________________________________________________________________
Duration of stress leakage (if applicable):
Duration of urge leakage (if applicable):
SELF REPORTED URINE LEAKAGE
Urine loss with:
|
Cough: |
Yes |
No |
|
Sneeze: |
Yes |
No |
|||
|
Laugh/giggle: |
Yes |
No |
|
Walk: |
Yes |
No |
|||
|
Run: |
Yes |
No |
|
Jump: |
Yes |
No |
|||
|
Downhill/steps: |
Yes |
No |
|
Lift/push/pull: |
Yes |
No |
|||
|
Change of position: |
Yes |
No |
|
Sexual intercourse: |
Yes |
No |
|||
|
With urge: |
Yes |
No |
|
Unconscious leakage: |
Yes |
No |
|||
|
Other (please give details): |
|||||||||
|
|
|||||||||
|
Nocturnal enuresis (bed wet when wakes): |
Yes |
No |
|
||||||
|
Association with menstrual cycle: |
Yes |
No |
Not applicable |
||||||
Frequency/urge triggers:
|
Running water: |
Yes |
No |
|
Cold weather: |
Yes |
No |
|
Key in lock: |
Yes |
No |
|
Change of positions: |
Yes |
No |
|
Other (please give details): |
||||||
Incontinence product(s): Yes No (if yes, give details below)
|
Type of product: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Amount of product: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Allowance received: |
|
|
|
|
|
|
Does leakage occur (tick one box only):
|
More than once a day? |
|
Not every day but more than twice a week? |
|
Not every week but more than twice a month? |
|
Less than once a month? |
What is the amount of each leak (tick more than on box if amount varies):
|
A drop or few drops? |
Enough to run down legs? |
|
Wets pants or pad? |
Bladder completely empties? |
|
Wets outer clothing? |
Leaking all the time? |
SELF REPORTED URINARY SYMPTOMS
|
Frequency (<2 hourly voids): |
Yes |
No |
|
|
Nocturia (>1 per night): |
Yes |
No |
|
|
Urgency: |
Yes |
No |
[If yes, continence therapists only: urge is imperative/suprapubic/urethral] |
|
|
|||
|
Able to defer void: |
Yes |
No |
If yes, how long? |
|
|
|||
|
Dysuria: |
Yes |
No |
|
|
Haematuria: |
Yes |
No |
|
|
Pain suggestive of urinary disorder: |
Yes |
No |
If yes, details: |
|
|
|||
|
History or UTI or cystitis: |
Yes |
No |
If yes, details (including frequency of episodes and treatment): |
|
|
|
|
|
SELF REPORTED VOIDING SYMPTOMS
Desire to void: Yes No Hesitancy: Yes No
Interrupted stream: Yes No Small voids: Yes No
Strain to void: Yes No Manual expression: Yes No
Revoid (<½ hr): Yes No Terminal dribbling: Yes No
URINARY HISTORY
History of incontinence:
Childhood: No Yes
Pregnancy: No Yes
Postnatal: No Yes
Previous conservative management:
Previous medical management:
Previous incontinence surgery:
Vaginal: procedure(s): ___________________ date(s): ___________________
Retropubic: procedure(s): ___________________ date(s): ___________________
Other: procedure(s): ___________________ date(s): ___________________
BOWEL HABIT
|
Usual bowel pattern: |
||||||||||
|
|
||||||||||
|
Use of laxatives/diet/other products (please circle and give details): |
||||||||||
|
|
||||||||||
|
|
||||||||||
|
Hold flatus: |
Yes |
No |
|
Urgency: |
Yes |
No |
|
Problems initiating: |
Yes |
No |
|
Problems completing: |
Yes |
No |
|
Straining: |
Yes |
No |
|
Perineal support: |
Yes |
No |
|
Manual evacuation: |
Yes |
No |
|
Soiling: |
Yes |
No |
|
Problems initiating: |
Yes |
No |
|
|
|
|
|
|
|
|
|
|
|
|
|
[Continence therapists only: details of voiding and defecation positions if relevant] |
||||||||||
|
|
||||||||||
|
|
||||||||||
OBSTETRIC HISTORY
|
No. of pregnancies >20/40: |
No. of pregnancies <20/40 (if relevant): |
|
|
|
||
|
Types of delivery, number, complications of note: |
||
|
|
||
|
Family completed? |
Yes No |
|
|
|
|
|
GYNAECOLOGICAL HISTORY
|
Cycle: |
LMP: |
|||
|
|
||||
|
Menopause: |
Yes |
No |
If yes, age ______ |
|
|
|
||||
|
Sexually active: |
Yes |
No |
If yes, contraception: |
|
|
|
||||
|
Dyspareunia: |
Yes |
No |
If yes, details: |
|
|
|
||||
|
Prolapse symptoms: |
Yes |
No |
If yes, details: |
|
|
|
||||
|
Normal smear history: |
Yes |
No |
If no, details: |
|
|
|
||||
|
Date of last smear: |
Mammography: |
|||
|
|
||||
|
Other: |
||||
GENERAL HEALTH
Medical history:
Glaucoma? Yes No
Surgical history (including gynaecological, excluding incontinence):
Family history:
Symptoms review:
CNS:
CVS:
RESP:
GIT:
MUSCULOSKELETAL:
Drugs and allergies:
Vaginal oestrogens? Yes No If yes, name and dosage
Hormone replacement therapy? Yes No If yes, name and dosage
Anticholinergics for urinary symptoms? Yes No If yes, name and dosage
LIFESTYLE
Occupation: Living circumstances:
Social activities: Exercise/activity/recreation:
Mobility (if impaired): Smoking: Yes No If yes, number per day:
Fluid intake (including type and amount of caffeine):
ETHNICITY (Please ask each woman to complete, or assist where appropriate)
Please tick as many boxes as you need to show which ethnic group(s) you belong to:
NZ Maori Samoan Cook Island Maori Other
NZ European or Pakeha Tongan Chinese
Other European Nuiean Indian
PHYSICAL EXAMINATION
|
Height (cm): |
Weight (kg): |
|
||||||||||||||
|
|
|
|||||||||||||||
|
CVS: |
BP: |
Pulse: |
Normal |
Abnormal, give details |
|
|
||||||||||
|
|
|
|||||||||||||||
|
|
|
|||||||||||||||
|
RESP: |
Normal |
Abnormal, give details |
|
|||||||||||||
|
|
|
|||||||||||||||
|
|
|
|||||||||||||||
|
NEURO: |
Lower limb power: |
Normal |
Abnormal, give details |
|
||||||||||||
|
|
Lower limb sensation: |
Normal |
Abnormal, give details |
|
||||||||||||
|
|
Lower limb reflexes: |
Normal |
Abnormal, give details |
|
||||||||||||
|
|
Anal/perineal sensation: |
Normal |
Abnormal, give details |
|
||||||||||||
|
|
Anal reflex: |
Normal |
Abnormal, give details |
|
||||||||||||
|
|
|
|||||||||||||||
|
|
|
|||||||||||||||
|
ABDOMINAL: |
Normal |
Abnormal, give details |
|
|||||||||||||
|
|
|
|||||||||||||||
|
|
|
|||||||||||||||
|
RECTAL: |
Normal |
Abnormal, give details |
|
|||||||||||||
|
|
|
|||||||||||||||
|
PELVIC: |
|
Nil |
Minimal |
Moderate |
Severe (please circle number) |
|
||||||||||
|
|
Atrophic changes: |
0 |
1 |
2 |
3 |
|
|
|
||||||||
|
|
|
|||||||||||||||
|
|
Prolapse: |
Nil |
Stage I |
Stage II |
Stage III |
Stage IV (please circle number) |
||||||||||
|
|
|
Urethrocele: |
0 |
1 |
2 |
3 |
4 |
|
|
|||||||
|
|
|
Cystocele: |
0 |
1 |
2 |
3 |
4 |
|
|
|||||||
|
|
|
Uterine: |
0 |
1 |
2 |
3 |
4 |
|
|
|||||||
|
|
|
Vault: |
0 |
1 |
2 |
3 |
4 |
|
|
|||||||
|
|
|
Enterocele: |
0 |
1 |
2 |
3 |
4 |
|
|
|||||||
|
|
|
Rectocele: |
0 |
1 |
2 |
3 |
4 |
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
Position in which examined: |
|
|
|
||||||||||||
|
|
|
|
|
|
||||||||||||
|
|
[KEY: Nil – no prolapse demonstrated with maximal valsalva; Stage I – most distal position of prolapse (DPP) >1cm above plane of hymen; Stage II – DPP <1cm above or below plane of hymen; Stage III – DPP >1cm below plane of hymen, but <2cm of total vaginal length; Stage IV – complete eversion of total vaginal length or lower genital tract] |
|
||||||||||||||
|
|
|
|||||||||||||||
|
|
Urethra: |
|
||||||||||||||
|
|
|
|||||||||||||||
|
|
Cervix: |
Smear taken: |
Yes No |
|
||||||||||||
|
|
|
|||||||||||||||
|
|
Uterus: |
|
|
|||||||||||||
|
|
|
|
|
|||||||||||||
|
|
Adenexae: |
|
|
|||||||||||||
|
|
|
|
|
|||||||||||||
|
|
Demonstrable leakage: |
Yes No |
|
|||||||||||||
|
|
|
|||||||||||||||
|
|
Voluntary pelvic floor muscle contraction: |
Yes No |
|
|||||||||||||
PHYSICAL EXAMINATION (CONTINENCE THERAPISTS ONLY)
|
Post void residual (ultrasound): |
||||||||
|
|
||||||||
|
Able to interrupt stream: |
Yes |
No change |
Slowed |
|
||||
|
|
||||||||
|
Perineal observation: |
||||||||
|
|
Movement with valsalva: |
None |
Minimal |
Ballooning |
Leakage |
|||
|
|
Movement with VPFMC: |
Cephalic |
Caudal |
Neither |
|
|||
|
|
Vaginal/urethral wink: |
Yes |
No |
|
|
|||
|
|
Anal wink: |
Yes |
No |
|
|
|||
|
|
||||||||
|
Palpation: |
||||||||
|
|
PFM symmetry at rest: |
|||||||
|
|
PFM symmetry with contraction: |
|||||||
|
|
||||||||
|
VPFMC: |
||||||||
|
|
Accompanied by: |
Breath holding |
Abdominals |
Gluteals |
Hip adductors |
|||
|
|
||||||||
|
|
Grade (please circle): |
0 |
Nil |
|||||
|
|
1 |
Flicker (with or without stretch) |
||||||
|
|
2 |
Weak (minimal lift or hold) |
||||||
|
|
3 |
Fair (definite lift) |
||||||
|
|
4 |
Good (definite lift and hold) |
||||||
|
|
5 |
Strong (good lift and hold, repeatable) |
||||||
|
|
|
|
||||||
|
|
Number of repetitions: |
|||||||
|
|
||||||||
|
|
Length of hold: |
|||||||
|
|
||||||||
|
|
Contraction with cough: |
Reflex |
Voluntary |
None |
||||
SUMMARY OF TESTS AND INVESTIGATIONS
MSSU:
Urinary diary (see attached):
24 hour home pad test:
Pre test pad weight: ______ g + ______ g + ______ g = ______ g
Post test pad weight: ______ g + ______ g + ______ g = ______ g
Total pad weight gain: ______ g
.cm
Transperineal ultrasound findings:
|
|
Bladder neck descent: |
Urodynamic findings:
|
|
Urodynamic stress incontinence: |
Yes |
No |
|
|
Intrinsic sphincter deficiency: |
Yes |
No |
|
|
Idiopathic detrusor overactivity: |
Yes |
No |
|
|
Voiding dysfunction: |
Yes |
No |
|
|
Other (please give details): |
||
SUMMARY
Problem list
__________________________________________________________________________________________
__________________________________________________________________________________________
__________________________________________________________________________________________
__________________________________________________________________________________________
__________________________________________________________________________________________
__________________________________________________________________________________________
__________________________________________________________________________________________
__________________________________________________________________________________________
Plan
__________________________________________________________________________________________
__________________________________________________________________________________________
__________________________________________________________________________________________
__________________________________________________________________________________________
__________________________________________________________________________________________
__________________________________________________________________________________________
__________________________________________________________________________________________
__________________________________________________________________________________________
__________________________________________________________________________________________
__________________________________________________________________________________________
__________________________________________________________________________________________
__________________________________________________________________________________________
CONTINENCE THERAPISTS ONLY
Informed consent for transperineal / vaginal / rectal examination (please delete if not appropriate)
|
|
|
|
|
|
|
Signature: |
|
|
Date: |
______/______/_______ |
|
|
(Client) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Signature: |
|
|
Date: |
______/______/_______ |
|
|
(Therapist) |
|
|
|
ODHB
44428 V1 Issued 22/08/2007 Page
IMPORTANT CONTACT NUMBERS THE COMMUNITY EQUIPMENT AND CONTINENCE SERVICE
International Consultation on Incontinence Questionnaire Urinary Incontinence Short Form
Tags: assessment clinical, female, clinical, history, assessment, continence
- FREQUENTLY ASKED QUESTIONS ON THE WORLD SOCIAL FORUM (PREPARED
- PRESSEINFORMATION INNOVATIVE VERPACKUNGSMETHODE GEWINNT B2BPREIS 3M SCOTCH FLEX&SEAL VERSANDROLLE
- GROUNDS FOR TERMINATION OR SUSPENSION OF YOUR IFP GRANT
- IMPROVING THE BUSINESS ENVIRONMENT THROUGH CONSTRUCTIVE DIALOGUE IN TIMORLESTE
- ANHÅLLAN OM MATCHÄNDRING VI ANHÅLLER OM MATCHÄNDRING PÅ GRUND
- PAÍS (ZONA) ENCUESTA STEPS AÑO HOJA DE
- SR ALCALDEPRESIDENTE DEL ILMO AYUNTAMIENTO DE LA VILLA DE
- CAUSE DELL’ESPANSIONE DELLA POPOLAZIONE IN ALTRE AREE TESI
- REPERTORIO N RACCOLTA N CONVENZIONE PER LATTUAZIONE DEL PIANO
- SNIIM – MANUAL DE USUARIO SECRETARÍA DE COMERCIO Y
- RZODKIEWKA JEST TO ROŚLINĄ ZALICZAJĄCA SIĘ DO RODZINY KAPUSTOWATE
- KAU THE DEPARTMENT OF EUROPEAN LANGUAGES WRITING 2
- SMATRAM DA TVRDNJA F6KOJA JE PO KLJUČU NETAČNA (F62)
- FRANÇAIS MORTGAGE BROKERAGES LENDERS AND ADMINISTRATORS ACT 2006 ONTARIO
- GUIA DE SITIOS INTERNET NACIONALES E INTERNACIONALES SOBRE ISO
- MEETING THE EMPLOYMENT TRANSPORTATION NEEDS OF PEOPLE WITH DISABILITIES
- GUIDANCE PHYSICAL COORDINATION FACTOR 2 – PHYSICAL COORDINATION SCOPE
- BACKGROUND PAPER SUBMITTED TO THE COMMITTEE ON INDIA
- RAJZ ÉS VIZUÁLIS KULTÚRA ALAPOZÓ ÉS FEJLESZTŐ SZAKASZ (5–8
- RECENT RESULT FROM CMD2 DETECTOR BORIS I KHAZIN
- NZQA EXPIRING UNIT STANDARD 8772 VERSION 7 PAGE 3
- ASSET THRESHOLDS AND SOCIAL PROTECTION A ‘THINKPIECE’ MICHAEL R
- UNCLASSIFIED CAREER BREAK SCHEME THIS INSTRUCTION APPLIES TO REFERENCE
- LEY 29493 DE IMPACTO AMBIENTAL PRESENTACION LA SUBSECRETARÍA
- FORMULARIO DE SOLICITUD DE USO DE VIVIENDA (SA
- OBSERVACIONES Y SUGERENCIAS BORRADOR DE OBSERVACIÓN GENERAL SOBRE EL
- 11 NATIVE AMERICAN PEOPLES A JOURNEY OF SELFDISCOVERY BOOK
- ZSE6124132021 OBWIESZCZENIE ZAWIADOMIENIE O WYDANIU DECYZJI NA PODSTAWIE ART
- MALE VICTIMS OF DOMESTIC ANDOR SEXUAL VIOLENCE FUND 201113
- TEMAS SUGERIDOS PARA LAS EXPOSICIONES EL ÉBOLA LOS CELULARES
ESCOLA DE SAÚDE PÚBLICA DO PARANÁ ESPP CURSO
 F UNCTIEBESCHRIJVING (TAKEN PROFIEL) PROJECTLEIDER OMGEVING 1IDENTIFICATIEGEGEVENS FUNCTIE
F UNCTIEBESCHRIJVING (TAKEN PROFIEL) PROJECTLEIDER OMGEVING 1IDENTIFICATIEGEGEVENS FUNCTIE TRAVERSING VIRTUALITY IN JANET CARDIFF’S COLORS OF SOUNDS BY
TRAVERSING VIRTUALITY IN JANET CARDIFF’S COLORS OF SOUNDS BY THE CLASSIC BIG BAND AND THE NOSTALGICS VOCAL QUARTET
THE CLASSIC BIG BAND AND THE NOSTALGICS VOCAL QUARTETORDENANZA NÚMERO 3081 VISTO EL EXPEDIENTE Nº 101962011 CD
NOTIFICATION FORM FOR SUSPECTED OUTBREAK OF INFECTIOUS DISEASE IN
CERVICAL SMEAR TEST A SUMMARY THE CERVICAL SMEAR
PIELIKUMS MINISTRU KABINETA 2016 GADA 20 SEPTEMBRA NOTEIKUMIEM NR
 POWERPLUSWATERMARKOBJECT283021517 FEDERAL CIRCUIT COURT OF AUSTRALIA REGISTRY FILE
POWERPLUSWATERMARKOBJECT283021517 FEDERAL CIRCUIT COURT OF AUSTRALIA REGISTRY FILEMIROSLAV VÁLEK DOMOV SÚ RUKY NA KTORÝCH SMIEŠ PLAKAŤ
7 MÁSTER OFICIAL DE DERECHO PRIVADO UNIVERSIDAD CARLOS III
NEIGHBOURHOOD PLANNING INDEPENDENT EXAMINATIONS WHO CAN CARRY OUT THE
 REGIONE SICILIANA COMUNE DI NASO PROVINCIA DI MESSINA PIANO
REGIONE SICILIANA COMUNE DI NASO PROVINCIA DI MESSINA PIANO ÄQUIVALENZTABELLE ORDNUNGEN 2006 UND AB WS 2014 STAND MAI
ÄQUIVALENZTABELLE ORDNUNGEN 2006 UND AB WS 2014 STAND MAI PETMCN H6 DDX3 101 NAME BERNARDO RODAMILANS DATE
PETMCN H6 DDX3 101 NAME BERNARDO RODAMILANS DATE HAVE SOMETHING DONE LOOK AT THIS EXAMPLE C
HAVE SOMETHING DONE LOOK AT THIS EXAMPLE CDNIA PIECZĘĆ NAGŁÓWKOWA WNIOSEK O NADANIE
DZIEŃ 11 LISTOPADA SCENARIUSZ SCENOGRAFIA I REKWIZYTY IMITACJA OGNISKA
EMPRESAS CADASTRADAS NA VIGILÂNCIA SANITÁRIA DE PORTO ALEGRE PARA
ZAŁĄCZNIK NR 3 UMOWA POWIERZENIA PRZETWARZANIA DANYCH OSOBOWYCH ZAWARTA